J Korean Soc Spine Surg.
2013 Dec;20(4):196-200. 10.4184/jkss.2013.20.4.196.
Atraumatic Spinal Interdural Hamatoma: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, National Police Hospital, Seoul, Korea. Xamxara@naver.com
- KMID: 1896950
- DOI: http://doi.org/10.4184/jkss.2013.20.4.196
Abstract
- STUDY DESIGN: A case report.
OBJECTIVES
To investigate the outcomes of recapping laminoplasty for the treatment of atraumatic spinal interdural hematoma. SUMMARY OF LITERATURE REVIEW: There are several causes for a spinal hematoma. The occurrence of spinal hematoma is rare; in particular, the ones arising atraumaticaly are considered extremely rare.
MATERIALS AND METHODS
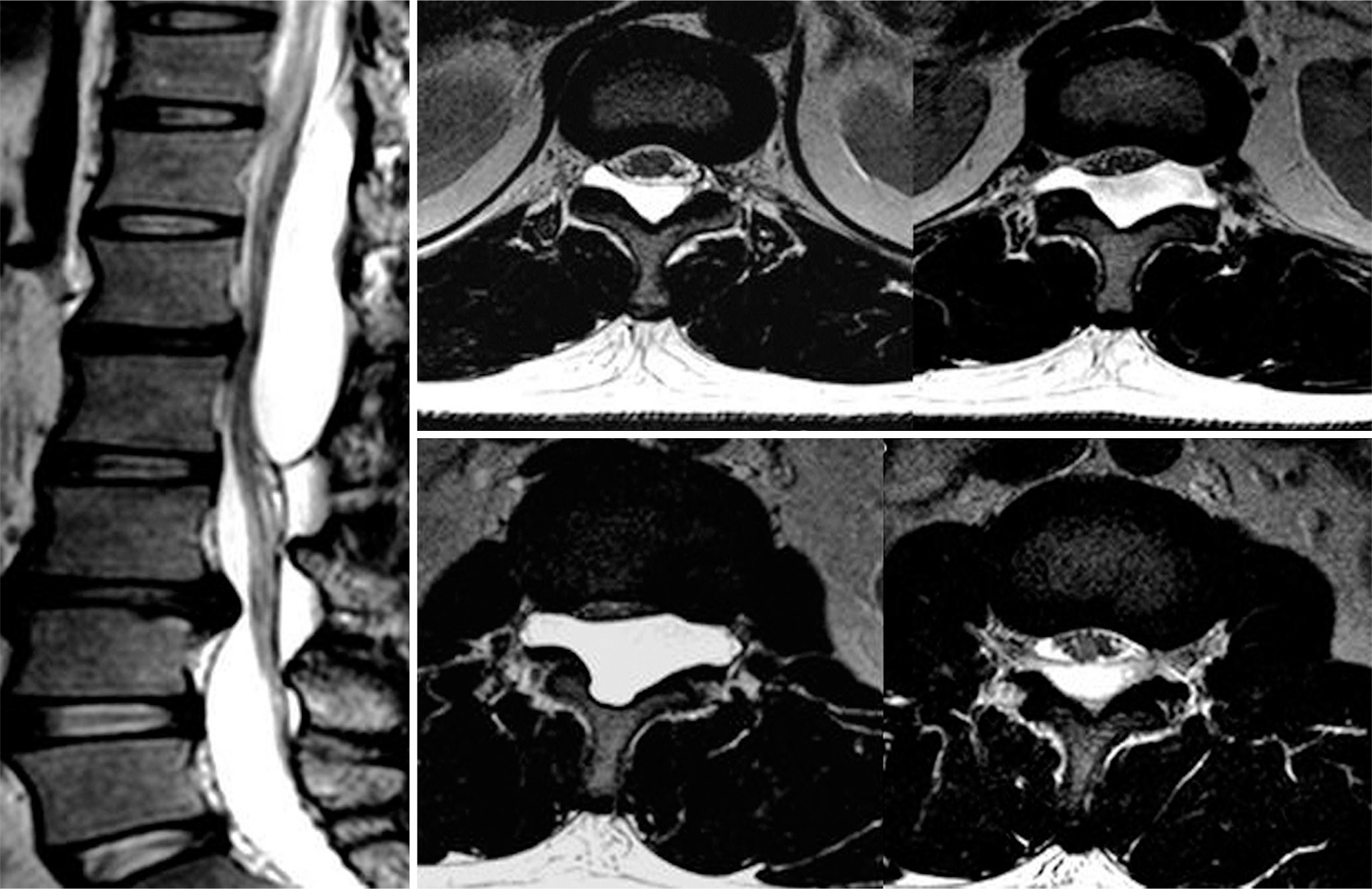
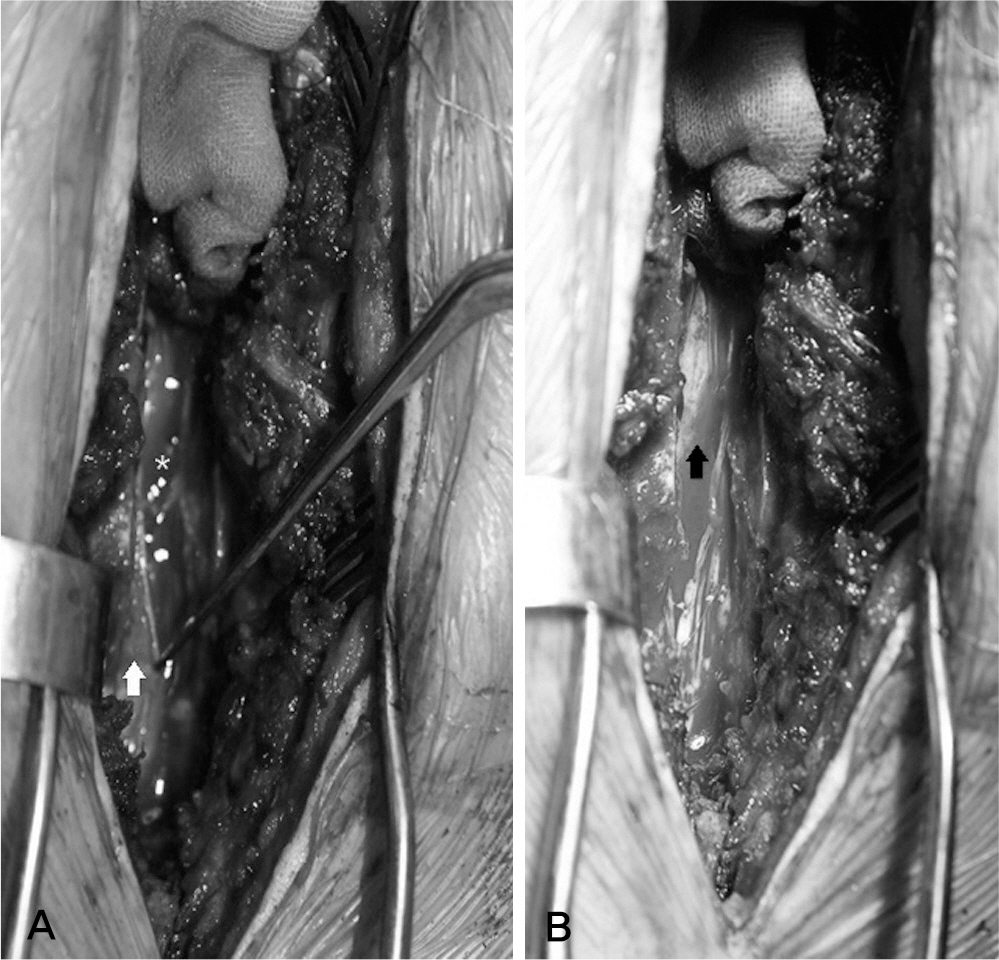
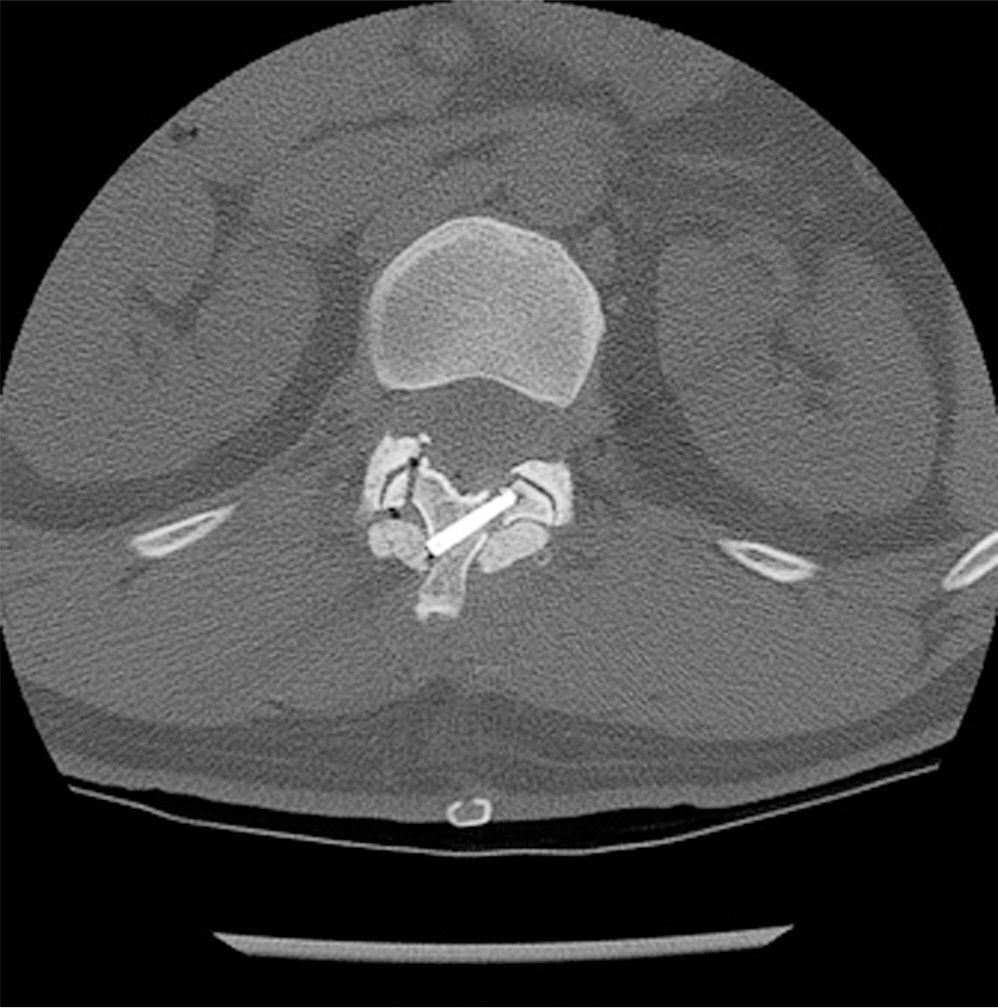
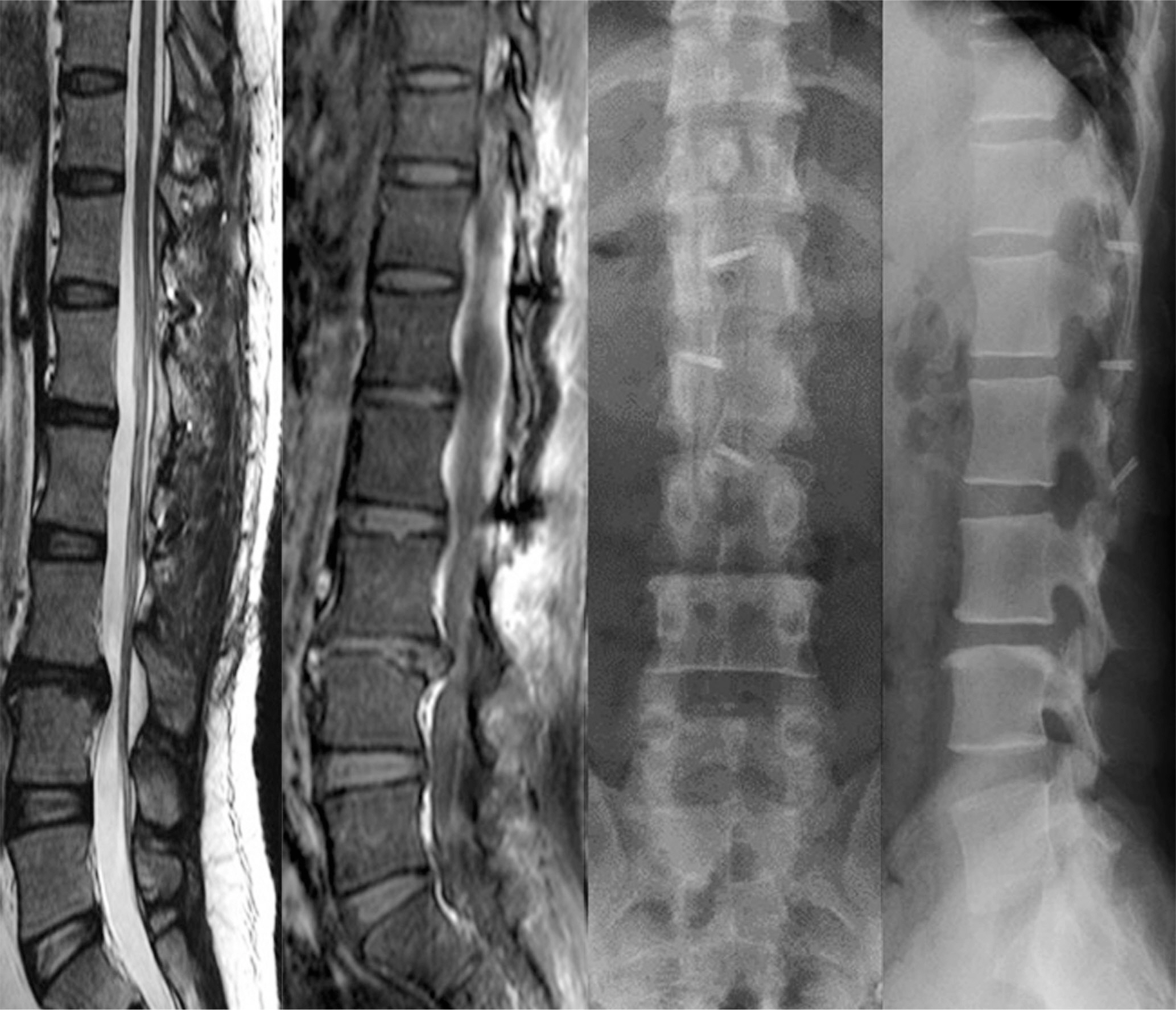
We studied a 33 year old male patient without any known risk factor. Magnetic resonance image has revealed an intraspinal epidural cyst compressing on the spinal nerve. After performing recapping laminoplasty, followed by partial excision of dura mater and resection of hematoma, we were able to observe another layer of dura mater, confirming the location of hematoma within two epidural layers, i.e., an interdural hematoma.
RESULTS
Performing recapping laminoplasty is a more effective and less invasive procedure for removing cyst than conventionally used laminectomy. Patients were found to have synostosis after three months post-op, and they have exhibited neither lumbosacral pain nor lower limb motor weakness after six months follow-up. There were no recurrences or complications reported on our study.
CONCLUSION
There are a few reported cases of atraumatic spinal interdural hematoma. Our study shows that performing pars osteotomy with recapping laminoplasty yield good clinical outcome for the treatment of atraumatic spinal interdural hematoma.
MeSH Terms
Figure
Reference
-
1. Avrahami E, Tadmor R, Ram Z, Feibel M, Itzhak Y. MR demonstration of spontaneous acute epidural hematoma of the thoracic spine. Neuroradiology. 1989; 31:89–92.
Article2. Post MJ, Becerra JL, Madsen PW, et al. Acute spinal subdural hematoma: MR and CT findings with pathologic correlates. Am J Neuroradiol. 1994; 15:1895–905.3. Haines DZ, Harkey HL, Al‐Mefty O. The “subdural” space: a new look at an outdated concept. Neurosurgery. 1993; 32:111–20.4. Blomberg RG. The lumbar subdural extraarachnoid space of humans: an anatomical study using spinaloscopy in au-topsy cases. Anesth Analg. 1987; 66:177–80.5. Lö vblad KO, Baumgartner RW, Zambaz BD, Remonda L, Ozdoba C, Schroth G. Nontraumatic spinal epidural hematomas. MR features. Acta Radiol. 1997; 38:8–13.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Atraumatic Aseptic Necrosis of Both Talus: A Case Report
- Atraumatic Avulsion Fracture of Calcaneal Tuberosity in a Patient with Peripheral Neuropathy: A Case Report
- Interdural Cyst of the Thoracolumbar Region
- Thoracic Interdural Aspergillus Abscess Causing Rapid Fatal Spondylitis in the Presence of Posterior Mediastinitis
- Spontaneous Herniation of the Thoracic Spinal Cord: A Case Report