Tuberc Respir Dis.
2009 Mar;66(3):225-229. 10.4046/trd.2009.66.3.225.
A Case of Churg-Strauss Syndrome with Diffuse Alveolar Hemorrhage Presenting as Acute Acalculous Cholecystitis
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University College of Medicine, Busan, Korea. parkhk@pusan.ac.kr
- KMID: 1846385
- DOI: http://doi.org/10.4046/trd.2009.66.3.225
Abstract
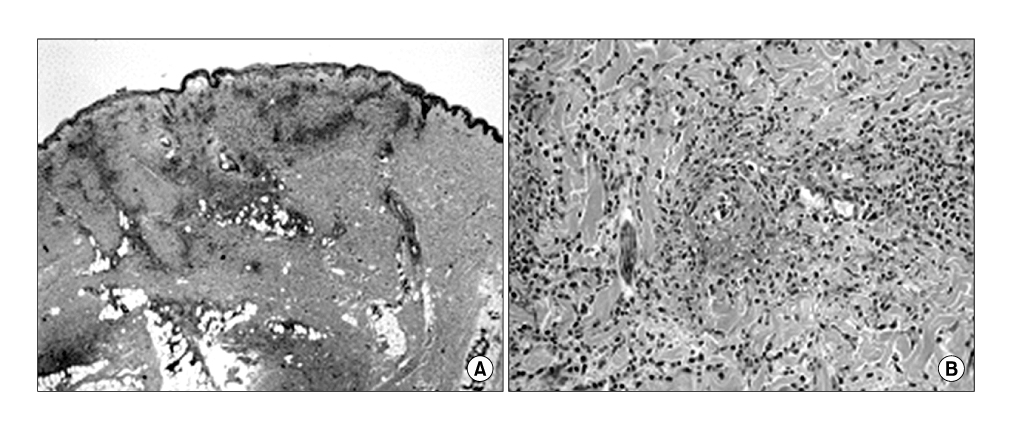
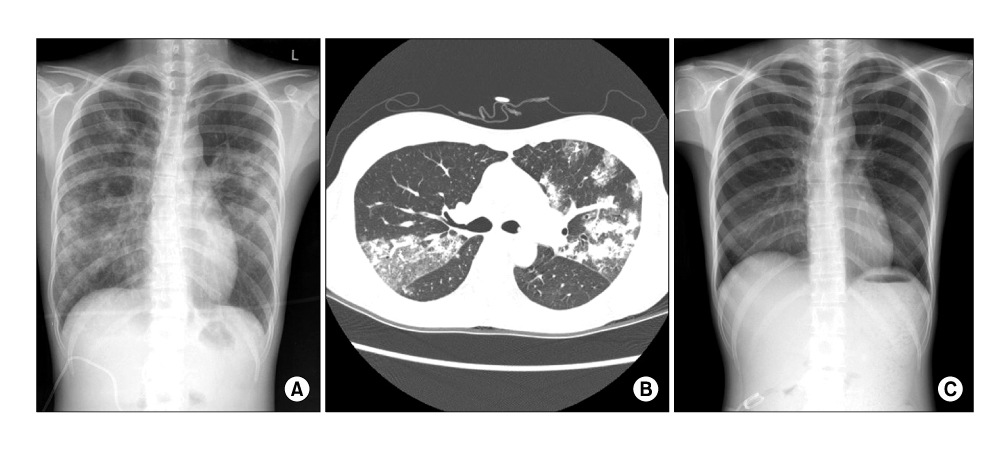
- Churg-Strauss syndrome (CSS) is a disorder that is characterized by asthma, hypereosinophilia and systemic vasculitis affecting a number of organs. The manifestations of acute cholecystitis and diffuse alveolar hemorrhage are rarely reported in CSS. A 22-year-old woman with bronchial asthma visited our hospital complaining of right upper quadrant pain with a sudden onset. The abdominal computed tomography (CT) scan revealed gall bladder edema consistent with acute cholecystitis. On the initial evaluation, marked hypereosinophilia was observed in the peripheral blood smear. The nerve conduction velocity measurements and a skin biopsy performed to confirm the organ involvement of disease indicated typical mononeuritis multiplex and necrotizing vasculitis, respectively, which was complicated with CSS. On the 12th hospital day, ground glass opacity and consolidations were newly developed on both lung fields. The bronchoalveolar lavage (BAL) fluid showed increasing bloody return in sequential aliquots that were characteristic of a diffuse alveolar hemorrhage. We report a case of CSS with acute cholecystitis and diffuse alveolar hemorrhage.
MeSH Terms
Figure
Cited by 1 articles
-
Churg-Strauss syndrome presenting as acute acalculous cholecystitis
Woo Joo Lee, Ji-Won Hwang, Eun Kim, Sehyo Yune, Jung Min Ha, Nara Yoon, Byung Jae Lee, Dong Chull Choi
Allergy Asthma Respir Dis. 2013;1(4):388-390. doi: 10.4168/aard.2013.1.4.388.
Reference
-
1. Churg J, Strauss L. Allergic granulomatosis, allergic angiitis and periarteritis nodosa. Am J Pathol. 1951. 27:277–301.2. Kurita M, Niwa Y, Hamada E, Hata Y, Oshima M, Mutoh H, et al. Churg-Strauss syndrome (allergic granulomatous angiitis) with multiple perforating ulcers of the small intestine, multiple ulcers of the colon, and mononeuritis multiplex. J Gastroenterol. 1994. 29:208–213.3. Suzuki M, Nabeshima K, Miyazaki M, Yoshimura H, Tagawa S, Shiraki K. Churg-Strauss syndrome complicated by colon erosion, acalculous cholecystitis and liver abscesses. World J Gastroenterol. 2005. 11:5248–5250.4. Nishie M, Tomiyama M, Kamijo M, Kannari K, Tanosaki M, Baba M, et al. Acute cholecystitis and duodenitis associated with Churg-Strauss syndrome. Hepatogastroenterology. 2003. 50:998–1002.5. Rolla G, Tartaglia N, Motta M, Ferrero N, Bergia R, Guida G, et al. Warning nonrespiratory symptoms in asthma: catastrophic abdominal involvement in a case of Churg-Strauss syndrome. Ann Allergy Asthma Immunol. 2007. 98:595–597.6. Tatsukawa H, Nagano S, Umeno Y, Oribe M. Churgstrauss syndrome with cholecystitis and renal involvement. Intern Med. 2003. 42:893–896.7. Jung SH, Kim KH, Nam SM, Park HC, Chu HK, Whang IS, et al. A case of Churg-Strauss syndrome with manifestations of esophageal ulcer, acute acalculous cholecystitis and ischemic colitis. Korean J Med. 1993. 45:369–375.8. Kim MS, Cho YJ, Roh SH. A case of Churg-Strauss syndrome which first presented as acute cholecystitis. J Asthma Allergy Clin Immunol. 2008. 28:143–147.9. Masi AT, Hunder GG, Lie JT, Michel BA, Bloch DA, Arend WP, et al. The American college of rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum. 1990. 33:1094–1100.10. Clutterbuck EJ, Pusey CD. Severe alveolar haemorrhage in Churg-Strauss syndrome. Eur J Respir Dis. 1987. 71:158–163.11. Lai RS, Lin SL, Lai NS, Lee PC. Churg-Strauss syndrome presenting with pulmonary capillaritis and diffuse alveolar hemorrhage. Scand J Rheumatol. 1998. 27:230–232.12. Schnabel A, Reuter M, Csernok E, Richter C, Gross WL. Subclinical alveolar bleeding in pulmonary vasculitides: correlation with indices of disease activity. Eur Respir J. 1999. 14:118–124.13. Yoshihara K, Arimura Y, Kobayashi O, Minoshima S, Kobayashi M, Yomogita S, et al. Clinical study on five myeloperoxidase specific anti-neutrophil cytoplasmic antibody (MPO-ANCA) positive Churg-Strauss syndrome cases. Ryumachi. 1998. 38:696–704.14. Franssen C, Gans R, Kallenberg C, Hageluken C, Hoorntje S. Disease spectrum of patients with antineutrophil cytoplasmic autoantibodies of defined specificity: distinct differences between patients with anti-proteinase 3 and anti-myeloperoxidase autoantibodies. J Intern Med. 1998. 244:209–216.15. Guillevin L, Lhote F, Gayraud M, Cohen P, Jarrousse B, Lortholary O, et al. Prognostic factors in polyarteritis nodosa and Churg-Strauss syndrome. A prospective study in 342 patients. Medicine (Baltimore). 1996. 75:17–28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Churg-Strauss Syndrome Which First Presented as Acute Cholecystitis
- Churg-Strauss syndrome presenting as acute acalculous cholecystitis
- A case of Churg-Strauss syndrome with manifestations of esophageal ulcer, acute acalculous cholecystitis and ischemic colitis
- Acalculous cholecystitis in a patient with Churg-Strauss syndrome
- Cholecystectomy of a patient with Churg-Strauss syndrome: A case report