J Korean Soc Spine Surg.
2014 Mar;21(1):15-23. 10.4184/jkss.2014.21.1.15.
Usefulness of Minimally Invasive Posterior Foraminotomy using Tubular Retractor for Lumbar Spinal Stenosis with Foraminal Stenosis
- Affiliations
-
- 1Department of Orthopedic Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. ch5420.choi@samsung.com
- KMID: 1840412
- DOI: http://doi.org/10.4184/jkss.2014.21.1.15
Abstract
- STUDY DESIGN: Retrospective study.
OBJECTIVES
The aim of this study was to report the usefulness of lumbar posterior foraminotomy and central decompression using tubular retractor with minimally invasive technique. SUMMARY OF LITERATURE REVIEW: Posterior decompression and arthrodesis for the treatment of lumbar spinal stenosis with foraminal stenosis is a classical surgical method. It is inappropriate for patients who have rejection to arthrodesis or medical problems, because it may have several complications.
MATERIALS AND METHODS
Clinical results were obtained from 12 patients who underwent posterior foraminotomy and central decompression from January 2009 to April 2011 and were assessed using a Visual analogue scale, Oswestry disability index and the Prolo outcome scale.
RESULTS
Six Of 12 patients showed immediate relief of radiculopathy. Postoperative posterior lumbar pain and spasm were negligible, and no surgically related complication was noted. During the follow-up period, the Oswestry disability index decreased from 24.25+/-2.89(pre-op) to 19.33+/-3.02(Last F/U)(p=0.28, paired t-test) in 8 of 12 patients.
CONCLUSIONS
A minimally invasive posterior foraminotomy and central decompression could be an alternative surgical option for the treatment of lumbar spinal stenosis with foraminal stenosis, especially in subjects with old age, having medical problems and refusal of arthrodesis.
MeSH Terms
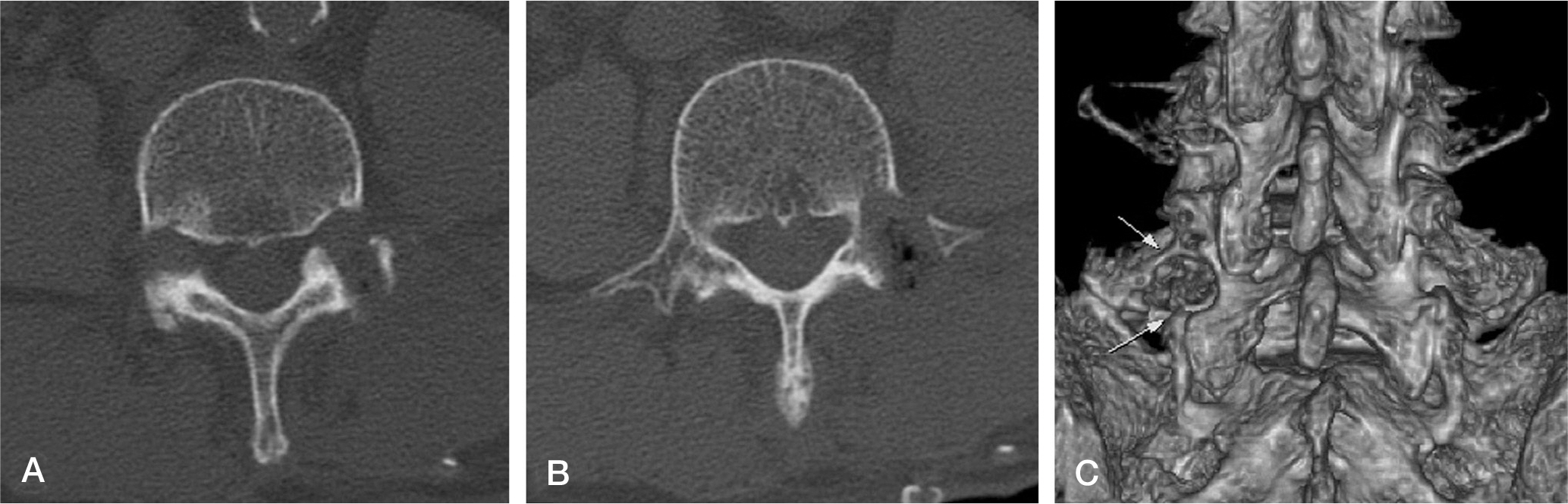
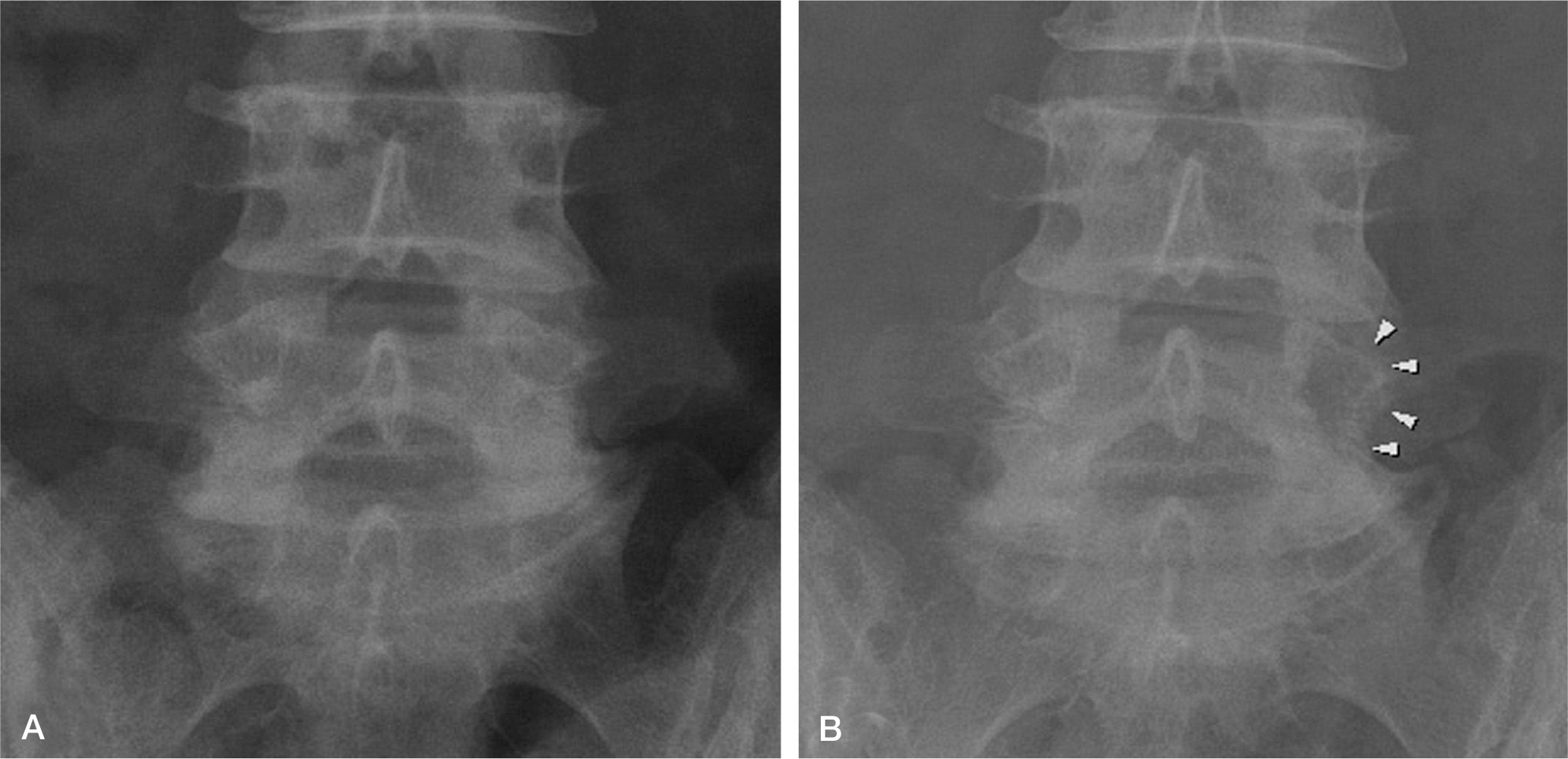
Figure
Reference
-
1. Crock HV. Normal and pathological anatomy of the lumbar spinal nerve root canals. J Bone Joint Surg Br. 1981; 63:487–90.
Article2. Hasegawa T, An HS, Haughton VM. Imaging anatomy of the lateral lumbar spinal canal. Semin Ultrasound CT MR. 1993; 14:404–13.
Article4. Cohen MS, Wall EJ, Brown RA, et al. 1990 AcroMed Award in basic science. Cauda equina anatomy. II: Ex-trathecal nerve roots and dorsal root ganglia. Spine. 1990; 15:1248–51.5. Hasue M, Kunogi J, Konno S, et al. Classification by position of dorsal root ganglia in the lumbosacral region. Spine (Phila Pa 1976). 1989; 14:1261–4.6. Vanderlinden RG. Subarticular entrapment of the dorsal root ganglion as a cause of sciatic pain. Spine (Phila Pa 1976). 1984; 9:19–22.
Article7. Weinstein J. Report of the 1985 ISSLS Traveling Fellowship. Mechanisms of spinal pain. The dorsal root ganglion and its role as a mediator of low-back pain. Spine (Phila Pa 1976). 1986; 11:999–1001.8. Wiltse LL, Guyer RD, Spencer CW, Glenn WV, Porter IS. Alar transverse process impingement of the L5 spinal nerve: the farout syndrome. Spine (Phila Pa 1976). 1984; 9:31–41.
Article9. Nathan H, Weizenbluth M, Halperin N. The lumbosacral ligament(LSL) with special emphasis on the “lumbosacral tunnel” and the entrapment of the 5th lumbar nerve. Int Orthop. 1982; 6:197–202.10. Burton CV, Kirkaldy-Willis WH, Yong-Hing K, et al. Cause of failure of surgery on the lumbar spine. Clin Orthop Relat Res. 1981; 157:191–9.11. Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003; 85:2089–92.
Article12. Cho KJ, Suk SI, Park SR, et al. Short fusion versus long fusion for degenerative lumbar scoliosis. Eur Spine J. 2008; 17:650–6.
Article13. Cassinelli EH, Eubanks J, Vogt M, Furey C, Yoo J, Bohlman HH. Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine (Phila Pa 1976). 2007; 32:230–5.14. Park HJ, Lee PE, Lee DK, Park HK. Postoperative complications in patients over 65 years of age with lumbar spinal stenosis and its Influencing factors. J Korean Soc Spine Surg. 2006; 13:114–9.
Article15. Matsui H, Tsuji H, Sekido H, Hirano N, Katoh Y, Maki-yama N. Results of expansive laminoplasty for lumbar spinal stenosis in active manual workers. Spine (Phila Pa 1976). 1992; 17(3 Suppl):S37–40.
Article16. Postacchini F, Cinotti G, Perugia D, Gumina S. The surgical treatment of central lumbar stenosis: multiple laminotomy compared with total laminectomy. J Bone Joint Surg Br. 1993; 75:386–92.
Article17. Postacchini F. Surgical management of lumbar spinal stenosis. Spine (Phila Pa 1976). 1999; 24:1043–7.
Article18. Sanderson PL, Getty CJ. Longterm results of partial under-cutting facetectomy for lumbar lateral recess stenosis. Spine (Phila Pa 1976). 1996; 21:1352–6.
Article19. Kim EH, Kim HT. En bloc partial laminectomy and posterior lumbar interbody fusion in foraminal spinal stenosis. Asian Spine J. 2009; 3:66–72.
Article20. Seong YJ, Lee JS, Suh KT, Kim JI, Lim JM, Goh TS. Posterior decompression and fusion in patients with multilevel lumbar foraminal stenosis: a comparison of segmental decompression and wide decompression. Asian Spine J. 2011; 5:100–6.
Article21. Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997; 3:301–7.22. Park YK, Kim JH, Chung HS, Suh JK. Microsurgical midline approach for the decompression of extraforaminal stenosis in L5-S1. J Neurosurg (Spine 3). 2003; 98:264–70.23. Kunogi J, Hasue M. Intrapedicular partial pediculectomy. OS Nos. 1994; 13:60–4.24. Fairbank J, Pynsent P. The Oswestry disability index. Spine (Phila Pa 1976). 2000; 25:2940–53.
Article25. Prolo DJ, Oklund SA, Butcher M. Toward uniformity in evaluating results of lumbar spine operations. A paradigm applied to posterior lumbar interbody fusions. Spine (Phila Pa 1976). 1986; 11:601–6.26. Getty CJ. Lumbar spinal stenosis: the clinical spectrum and the results of operation. J Bone Joint Surg. 1980; 62:481–5.
Article27. Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Influence of bone mineral density on pedicle screw fixation: A study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J. 2001; 1:402–7.28. Niggemeyer O, Strauss JM, Schulitz KP. Comparison of surgical procedures for degenerative lumbar spinal stenosis: a meta-analysis of the literature from 1975 to 1995. Eur Spine J. 1997; 6:423–9.
Article29. Hejazi N, Witzmann A, Hergan K, Hassler W. Combined transarticular lateral and medial approach with partial facetectomy for lumbar foraminal stenosis. Technical note. 2002; 96(1 Suppl):118–21.
Article30. You JW, Sohn HM, Lee JY, Yang KH. Comparison of the results of the decompression methods for degenerative lumbar spinal stenosis: comparison of posterior element saving procedures. J Korean Soc Spine Surg. 2005; 12:324–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Study of the Differences in Radiologic Results for Percutaneous Endoscopic Lumbar Foraminotomy and Microscopic or Micro-endoscopic Lumbar Foraminotomy
- Minimally Invasive Combined Interlaminar and Paraisthmic Approach for Symptomatic Lumbar Foraminal Stenosis : Surgical Technique and Preliminary Results
- Early Surgical Results of Minimally Invasive Posterior Foraminotomy using Tubular Retractor for Cervical Radiculopathy
- Clinical Applications of the Tubular Retractor on Spinal Disorders
- Fully Endoscopic Transforaminal Approach for L5–S1 Foraminal Stenosis: A Narrative Review