J Korean Surg Soc.
2011 Apr;80(4):260-266. 10.4174/jkss.2011.80.4.260.
Prognostic implication of metastatic lymph node ratio in node-positive rectal cancer
- Affiliations
-
- 1Department of Surgery, Dong-A University Medical Center, Busan, Korea. colonch@donga.ac.kr
- 2Department of Hemato-Oncology, Dong-A University Medical Center, Busan, Korea.
- 3Department of Pathology, Dong-A University Medical Center, Busan, Korea.
- 4Department of Radiation Oncology, Dong-A University Medical Center, Busan, Korea.
- 5Department of Statistics, Pusan National University College of Natural Sciences, Busan, Korea.
- KMID: 1820016
- DOI: http://doi.org/10.4174/jkss.2011.80.4.260
Abstract
- PURPOSE
The aim of this study was to evaluate the prognostic significance of the ratio between metastatic and examined lymph nodes (LNs) in patients with stage III rectal cancer.
METHODS
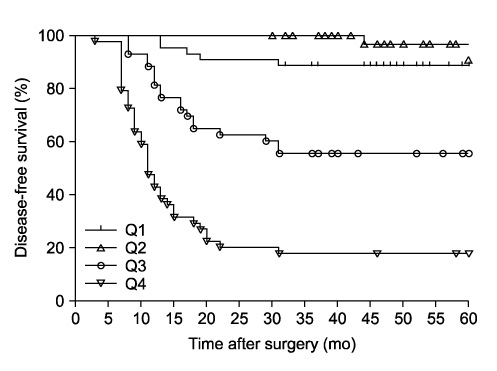
A review was made of 175 (male, 98) patients with stage III rectal cancer of R0 resection. LN disease was stratified both by the American Joint Committee on Cancer/International Union Against Cancer nodal classification (pN) and by quartiles of the lymph node ratio (LNR). Disease-free survivals (DFS) were made using Kaplan-Meier curves and assessed by the log rank test and multivariate analysis was performed using the Cox proportional hazards model.
RESULTS
Patients ranged in age from 29 to 83 (median, 60) years with median follow-up of 47 months (range, 13 to 181 months). months. There was a significant correlation between the number of metastatic LNs and the LNR (r = 0.8681, P < 0.0001). Cut-off points of LNR quartiles best to separate patients with regard to 5-year DFS were between quartile 2 and 3, and between 3 and 4 (LNR1, 2, and 3); the 5-year DFS according to such stratification was 89.6%, 55.8%, and 18.2% in LNR1, 2, and 3, respectively (P < 0.0001). Cox model identified the LNR as the most significant independent prognostic covariate; LNR2 showed 3.6 times (95% confidence interval [CI], 1.682 to 7.584; P = 0.0009) and LNR3, 18.7 times (95% CI, 6.872 to 50.664; P < 0.0001) more risky than LNR1.
CONCLUSION
This study suggests that ratio-based LN staging, which reflects the number of LNs examined and the quality of LN dissection, is a simple and reliable system for prognostic LN stratification in patients with stage III rectal cancer.
MeSH Terms
Figure
Reference
-
1. Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg. 1998. 133:894–899.2. Havenga K, Enker WE, Norstein J, Moriya Y, Heald RJ, van Houwelingen HC, et al. Improved survival and local control after total mesorectal excision or D3 lymphadenectomy in the treatment of primary rectal cancer: an international analysis of 1411 patients. Eur J Surg Oncol. 1999. 25:368–374.3. Law WL, Chu KW. Anterior resection for rectal cancer with mesorectal excision: a prospective evaluation of 622 patients. Ann Surg. 2004. 240:260–268.4. Kapiteijn E, Putter H, van de Velde CJ. Cooperative investigators of the Dutch ColoRectal Cancer Group. Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg. 2002. 89:1142–1149.5. Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al. AJCC cancer staging manual. 2002. 6th ed. New York: Springer-Verlag.6. Tepper JE, O'Connell MJ, Niedzwiecki D, Hollis D, Compton C, Benson AB 3rd, et al. Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol. 2001. 19:157–163.7. Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol. 2003. 21:2912–2919.8. Joseph NE, Sigurdson ER, Hanlon AL, Wang H, Mayer RJ, MacDonald JS, et al. Accuracy of determining nodal negativity in colorectal cancer on the basis of the number of nodes retrieved on resection. Ann Surg Oncol. 2003. 10:213–218.9. Goldstein NS, Sanford W, Coffey M, Layfield LJ. Lymph node recovery from colorectal resection specimens removed for adenocarcinoma. Trends over time and a recommendation for a minimum number of lymph nodes to be recovered. Am J Clin Pathol. 1996. 106:209–216.10. Wong JH, Severino R, Honnebier MB, Tom P, Namiki TS. Number of nodes examined and staging accuracy in colorectal carcinoma. J Clin Oncol. 1999. 17:2896–2900.11. Lee HY, Choi HJ, Park KJ, Shin JS, Kwon HC, Roh MS, et al. Prognostic significance of metastatic lymph node ratio in node-positive colon carcinoma. Ann Surg Oncol. 2007. 14:1712–1717.12. Berger AC, Sigurdson ER, LeVoyer T, Hanlon A, Mayer RJ, Macdonald JS, et al. Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol. 2005. 23:8706–8712.13. Peng J, Xu Y, Guan Z, Zhu J, Wang M, Cai G, et al. Prognostic significance of the metastatic lymph node ratio in node-positive rectal cancer. Ann Surg Oncol. 2008. 15:3118–3123.14. Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery--the clue to pelvic recurrence? Br J Surg. 1982. 69:613–616.15. Swanson RS, Compton CC, Stewart AK, Bland KI. The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. Ann Surg Oncol. 2003. 10:65–71.16. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma. 2nd English ed. Gastric Cancer. 1998. 1:10–24.17. Saito H, Fukumoto Y, Osaki T, Yamada Y, Fukuda K, Tatebe S, et al. Prognostic significance of the ratio between metastatic and dissected lymph nodes (n ratio) in patients with advanced gastric cancer. J Surg Oncol. 2008. 97:132–135.18. Persiani R, Rausei S, Biondi A, Boccia S, Cananzi F, D'Ugo D. Ratio of metastatic lymph nodes: impact on staging and survival of gastric cancer. Eur J Surg Oncol. 2008. 34:519–524.19. Kodera Y, Yamamura Y, Shimizu Y, Torii A, Hirai T, Yasui K, et al. Lymph node status assessment for gastric carcinoma: is the number of metastatic lymph nodes really practical as a parameter for N categories in the TNM Classification? Tumor Node Metastasis. J Surg Oncol. 1998. 69:15–20.20. Inoue K, Nakane Y, Iiyama H, Sato M, Kanbara T, Nakai K, et al. The superiority of ratio-based lymph node staging in gastric carcinoma. Ann Surg Oncol. 2002. 9:27–34.21. Nitti D, Marchet A, Olivieri M, Ambrosi A, Mencarelli R, Belluco C, et al. Ratio between metastatic and examined lymph nodes is an independent prognostic factor after D2 resection for gastric cancer: analysis of a large European monoinstitutional experience. Ann Surg Oncol. 2003. 10:1077–1085.22. Bando E, Yonemura Y, Taniguchi K, Fushida S, Fujimura T, Miwa K. Outcome of ratio of lymph node metastasis in gastric carcinoma. Ann Surg Oncol. 2002. 9:775–784.23. Megale Costa LJ, Soares HP, Gaspar HA, Trujillo LG, Santi PX, Pereira RS, et al. Ratio between positive lymph nodes and total dissected axillaries lymph nodes as an independent prognostic factor for disease-free survival in patients with breast cancer. Am J Clin Oncol. 2004. 27:304–306.24. Berger AC, Watson JC, Ross EA, Hoffman JP. The metastatic/examined lymph node ratio is an important prognostic factor after pancreaticoduodenectomy for pancreatic adenocarcinoma. Am Surg. 2004. 70:235–240.25. Herr HW. Superiority of ratio based lymph node staging for bladder cancer. J Urol. 2003. 169:943–945.26. Kim YS, Kim JH, Yoon SM, Choi EK, Ahn SD, Lee SW, et al. Lymph node ratio as a prognostic factor in patients with stage III rectal cancer treated with total mesorectal excision followed by chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2009. 74:796–802.27. Peschaud F, Benoist S, Julié C, Beauchet A, Penna C, Rougier P, et al. The ratio of metastatic to examined lymph nodes is a powerful independent prognostic factor in rectal cancer. Ann Surg. 2008. 248:1067–1073.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Implication of Lateral Pelvic Lymph Node Metastasis in Rectal Cancer Treated with Neoadjuvant Chemoradiotherapy
- Prognostic value of the lymph node metastasis in patients with ampulla of Vater cancer after surgical resection
- A Distribution Weighted Prognostic Scoring Model for Node Status in Advanced Rectal Cancer
- Clinical Implications of Lymph Node Metastasis in Colorectal Cancer: Current Status and Future Perspectives
- Lymph Node Metastases of Prostatic Adenocarcinoma in the Mesorectum in Patients with Rectal Cancer