Diabetes Metab J.
2015 Apr;39(2):137-146. 10.4093/dmj.2015.39.2.137.
Low Economic Status Is Identified as an Emerging Risk Factor for Diabetes Mellitus in Korean Men Aged 30 to 59 Years in Korean National Health and Nutrition Examination Survey 2008 to 2010
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. mkmoon@snu.ac.kr
- 2Department of Internal Medicine, Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1805897
- DOI: http://doi.org/10.4093/dmj.2015.39.2.137
Abstract
- BACKGROUND
We compared the association between economic status and the prevalence of diabetes mellitus (DM) using large nationwide datasets covering the previous 10 years in Korea.
METHODS
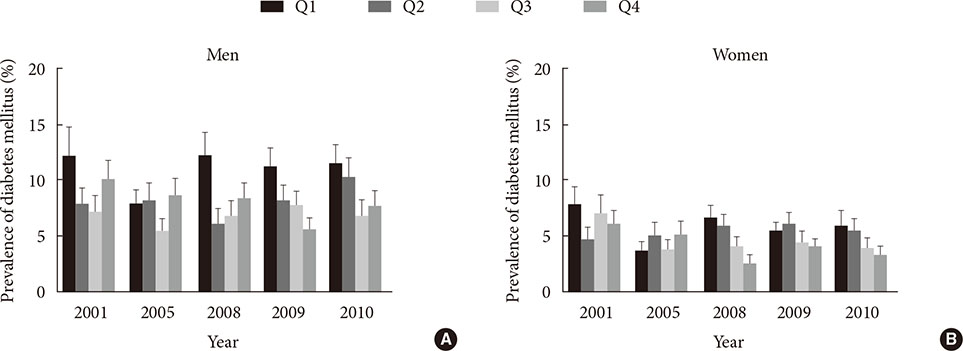
We analyzed the association between economic status and DM using Korean National Health and Nutrition Examination Survey (KNHANES) data from 2001 to 2010 weighted to represent the Korean population between 30 and 59 years of age. The economic status of participants was classified into quartiles according to monthly family income with an equivalence scale.
RESULTS
In men, the prevalence of diabetes in the lowest income quartile (Q1) was significantly higher than that in the other quartiles in 2008 (age and body mass index-adjusted odds ratio [OR], 1.846; 95% confidence interval [CI], 1.126 to 3.027; P=0.015), 2009 (OR, 1.706; 95% CI, 1.094 to 2.661; P=0.019), and 2010 (OR, 1.560; 95% CI, 1.024 to 2.377; P=0.039) but not in 2001 or 2005. The data indicated that classification in the lowest economic status was an independent risk factor for diabetes even after adjusting for abdominal obesity, dyslipidemia, hypertension and education level in men of KNHANES 2008 to 2010. Although economic status was significantly associated with abdominal obesity, hypertriglyceridemia, and hypertension in women (P<0.001), there was no significant association between economic status and DM in women.
CONCLUSION
Korean men between 30 and 59 years of age with the lowest economic status had a significantly higher prevalence of DM in 2008 to 2010 even after adjusting for other risk factors.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Lower Leg Fat Depots Are Associated with Albuminuria Independently of Obesity, Insulin Resistance, and Metabolic Syndrome (Korea National Health and Nutrition Examination Surveys 2008 to 2011)
Eugene Han, Nan Hee Cho, Mi Kyung Kim, Hye Soon Kim
Diabetes Metab J. 2019;43(4):461-473. doi: 10.4093/dmj.2018.0081.
Reference
-
1. Kim SH. International statistics yearbook. 16th ed. Daejeon: Statistics Korea;2011.2. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011; 35:303–308.3. Ning F, Pang ZC, Dong YH, Gao WG, Nan HR, Wang SJ, Zhang L, Ren J, Tuomilehto J, Hammar N, Malmberg K, Andersson SW, Qiao Q. Qingdao Diabetes Survey Group. Risk factors associated with the dramatic increase in the prevalence of diabetes in the adult Chinese population in Qingdao, China. Diabet Med. 2009; 26:855–863.4. Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J. China National Diabetes and Metabolic Disorders Study Group. Prevalence of diabetes among men and women in China. N Engl J Med. 2010; 362:1090–1101.5. Shen J, Goyal A, Sperling L. The emerging epidemic of obesity, diabetes, and the metabolic syndrome in china. Cardiol Res Pract. 2012; 2012:178675.6. Ramachandran A, Snehalatha C, Vijay V. Temporal changes in prevalence of type 2 diabetes and impaired glucose tolerance in urban southern India. Diabetes Res Clin Pract. 2002; 58:55–60.7. Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and type 2 diabetes in African American and non-Hispanic white women and men: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health. 2001; 91:76–83.8. Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J Psychosom Res. 2002; 53:891–895.9. Rabi DM, Edwards AL, Southern DA, Svenson LW, Sargious PM, Norton P, Larsen ET, Ghali WA. Association of socio-economic status with diabetes prevalence and utilization of diabetes care services. BMC Health Serv Res. 2006; 6:124.10. Pan XR, Yang WY, Li GW, Liu J. National Diabetes Prevention and Control Cooperative Group. Prevalence of diabetes and its risk factors in China, 1994. Diabetes Care. 1997; 20:1664–1669.11. Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, Rao PV, Yajnik CS, Prasanna Kumar KM, Nair JD. Diabetes Epidemiology Study Group in India (DESI). High prevalence of diabetes and impaired glucose tolerance in India: national urban diabetes survey. Diabetologia. 2001; 44:1094–1101.12. Mohan V, Shanthirani S, Deepa R, Premalatha G, Sastry NG, Saroja R. Chennai Urban Population Study (CUPS No. 4). Intra-urban differences in the prevalence of the metabolic syndrome in southern India: the Chennai Urban Population Study (CUPS No. 4). Diabet Med. 2001; 18:280–287.13. Deepa M, Anjana RM, Manjula D, Narayan KM, Mohan V. Convergence of prevalence rates of diabetes and cardiometabolic risk factors in middle and low income groups in urban India: 10-year follow-up of the Chennai Urban Population Study. J Diabetes Sci Technol. 2011; 5:918–927.14. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009; 32:2016–2020.15. Koo BK, Kim EK, Choi H, Park KS, Moon MK. Decreasing trends of the prevalence of diabetes and obesity in Korean women aged 30-59 years over the past decade: results from the Korean National Health and Nutrition Examination Survey, 2001-2010. Diabetes Care. 2013; 36:e95–e96.16. Armitage P, Colton T. Chapter, Software for sample survey data, misuse of standard packages. Encyclopedia of biostatistics. New York: John Wiley & Sons;1998. p. 4167–4174.17. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F. American Heart Association. National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112:2735–2752.18. Bassett J. International Diabetes Institute. World Health Organization Regional Office for the Western Pacific. International Association for the Study of Obesity. International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. Australia: Health Communications Australia;2000.19. Korea Centers for Disease Control and Prevention. The Korean National Health and Nutrition Examination Survey. Cheongju: Korea Centers for Disease Control and Prevention;2010.20. Korea Centers for Disease Control and Prevention. The Korean National Health and Nutrition Examination Survey. Cheongju: Korea Centers for Disease Control and Prevention;2005.21. Korea Centers for Disease Control and Prevention. The Korean National Health and Nutrition Examination Survey. Cheongju: Korea Centers for Disease Control and Prevention;2001.22. Toth MJ, Tchernof A, Sites CK, Poehlman ET. Menopause-related changes in body fat distribution. Ann N Y Acad Sci. 2000; 904:502–506.23. Poehlman ET, Toth MJ, Gardner AW. Changes in energy balance and body composition at menopause: a controlled longitudinal study. Ann Intern Med. 1995; 123:673–675.24. Eshtiaghi R, Esteghamati A, Nakhjavani M. Menopause is an independent predictor of metabolic syndrome in Iranian women. Maturitas. 2010; 65:262–266.25. Bosma H, Schrijvers C, Mackenbach JP. Socioeconomic inequalities in mortality and importance of perceived control: cohort study. BMJ. 1999; 319:1469–1470.26. Kunst AE, Groenhof F, Mackenbach JP, Health EW. Occupational class and cause specific mortality in middle aged men in 11 European countries: comparison of population based studies. EU Working Group on Socioeconomic Inequalities in Health. BMJ. 1998; 316:1636–1642.27. van Lenthe FJ, Schrijvers CT, Droomers M, Joung IM, Louwman MJ, Mackenbach JP. Investigating explanations of socio-economic inequalities in health: the Dutch GLOBE study. Eur J Public Health. 2004; 14:63–70.28. Klein-Hesselink DJ, Spruit IP. The contribution of unemployment to socioeconomic health differences. Int J Epidemiol. 1992; 21:329–337.29. Schrijvers CT, van de Mheen HD, Stronks K, Mackenbach JP. Socioeconomic inequalities in health in the working population: the contribution of working conditions. Int J Epidemiol. 1998; 27:1011–1018.30. Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008; 31:2383–2390.31. Campayo A, de Jonge P, Roy JF, Saz P, de la Camara C, Quintanilla MA, Marcos G, Santabarbara J, Lobo A. ZARADEMP Project. Depressive disorder and incident diabetes mellitus: the effect of characteristics of depression. Am J Psychiatry. 2010; 167:580–588.32. Pouwer F, Kupper N, Adriaanse MC. Does emotional stress cause type 2 diabetes mellitus? A review from the European Depression in Diabetes (EDID) Research Consortium. Discov Med. 2010; 9:112–118.33. Kumari M, Head J, Marmot M. Prospective study of social and other risk factors for incidence of type 2 diabetes in the Whitehall II study. Arch Intern Med. 2004; 164:1873–1880.34. Heraclides A, Chandola T, Witte DR, Brunner EJ. Psychosocial stress at work doubles the risk of type 2 diabetes in middle-aged women: evidence from the Whitehall II study. Diabetes Care. 2009; 32:2230–2235.35. Lee HJ, Kim MG, Noe DM, Kang SH, Son BD, Ryu JY, Lim YS. The structure of poverty in Korea. Seoul: Korea Institute for Health and Social Welfare;2006.36. Khang YH, Lynch JW, Yun S, Lee SI. Trends in socioeconomic health inequalities in Korea: use of mortality and morbidity measures. J Epidemiol Community Health. 2004; 58:308–314.37. Khang YH, Kim HR. Explaining socioeconomic inequality in mortality among South Koreans: an examination of multiple pathways in a nationally representative longitudinal study. Int J Epidemiol. 2005; 34:630–637.38. Lim H, Nguyen T, Choue R, Wang Y. Sociodemographic disparities in the composition of metabolic syndrome components among adults in South Korea. Diabetes Care. 2012; 35:2028–2035.39. Marra CA, Lynd LD, Esdaile JM, Kopec J, Anis AH. The impact of low family income on self-reported health outcomes in patients with rheumatoid arthritis within a publicly funded health-care environment. Rheumatology (Oxford). 2004; 43:1390–1397.40. Sculpher MJ, O'Brien BJ. Income effects of reduced health and health effects of reduced income: implications for health-state valuation. Med Decis Making. 2000; 20:207–215.41. Rhee SY, Chon S, Kwon MK, Park Ie B, Ahn KJ, Kim IJ, Kim SH, Lee HW, Koh KS, Kim DM, Baik SH, Lee KW, Nam MS, Park YS, Woo JT, Kim YS. Prevalence of chronic complications in korean patients with type 2 diabetes mellitus based on the korean national diabetes program. Diabetes Metab J. 2011; 35:504–512.42. Choi YJ, Cho YM, Park CK, Jang HC, Park KS, Kim SY, Lee HK. Rapidly increasing diabetes-related mortality with socio-environmental changes in South Korea during the last two decades. Diabetes Res Clin Pract. 2006; 74:295–300.43. Caiazzo A, Cardano M, Cois E, Costa G, Marinacci C, Spadea T, Vannoni F, Venturini L. Inequalities in health in Italy. Epidemiol Prev. 2004; 28:3 Suppl. 1–161.44. Guize L, Jaffiol C, Gueniot M, Bringer J, Giudicelli C, Tramoni M, Thomas F, Pannier B, Bean K, Jego B. Diabetes and socio-economic deprivation. A study in a large French population. Bull Acad Natl Med. 2008; 192:1707–1723.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in the management of hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the COVID-19 pandemic: data from the 2010-2020 Korea National Health and Nutrition Examination Survey
- Relationship between Diabetes Mellitus and Anemia in Korean Adults-Based on the Korean National Health and Nutritional Examination Survey VI
- The Presence of Diabetes Mellitus and Anemia in Korean Adults-based on data from 2005 Korean National Health and Nutrition Examination Survey (KNHANES III)
- Association between cigarette smoking status and periodontal disease in adults: results from the 2012 Korea national health and nutrition examination survey
- Fundus Examination Rate in Diabetics and the Public Health Factors Associated With Fundus Examination Rate