Yonsei Med J.
2010 Jul;51(4):599-601. 10.3349/ymj.2010.51.4.599.
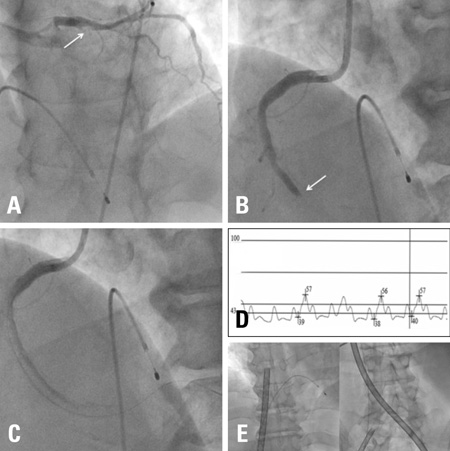
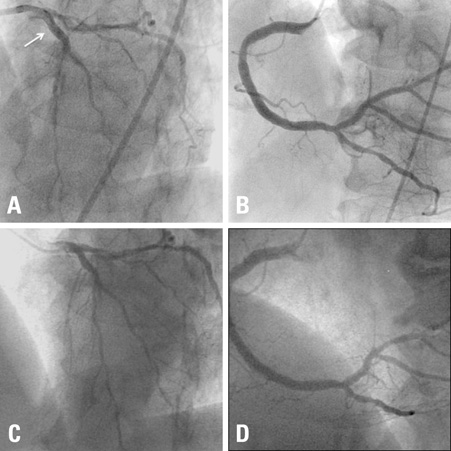
Percutaneous Cardiopulmonary Support in Refractory No-Reflow with Cardiogenic Shock after Coronary Stenting in Acute Myocardial Infarction
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. kjs1218@yuhs.ac
- KMID: 1805202
- DOI: http://doi.org/10.3349/ymj.2010.51.4.599
Abstract
- Coronary no-reflow is defined as inadequate myocardial perfusion of a given coronary segment without angiographic evidence of mechanical vessel obstruction. No-reflow is visualized angiographically as a reduction in thrombolysis in myocardial infarction (TIMI) flow grade and is typically accompanied by chest pain, electrocardiographic changes with ST-segment shift and possible hemodynamic compromise. No-reflow during primary percutaneous coronary intervention (PCI) results in increasing mortality and morbidity. Therefore, treatment of noreflow is associated with improved clinical outcomes. Generally, the treatment of no-reflow is based on pharmacotherapy. In this case, despite maximal pharmacotherapy and intraaortic balloon pump (IABP), refractory no-reflow accompanied with cardiogenic shock was successfully treated with percutaneous cardiopulmonary support (PCPS).
Figure
Reference
-
1. Lee CH, Wong HB, Tan HC, Zhang JJ, Teo SG, Ong HY, et al. Impact of reversibility of no reflow phenomenon on 30-day mortality following percutaneous revascularization for acute myocardial infarction-insights from a 1,328 patient registry. J Interv Cardiol. 2005. 18:261–266.
Article2. Piana RN, Paik GY, Moscucci M, Cohen DJ, Gibson CM, Kugelmass AD, et al. Incidence and treatment of 'no-reflow' after percutaneous coronary intervention. Circulation. 1994. 89:2514–2518.3. van Gaal WJ, Banning AP. Percutaneous coronary intervention and the no-reflow phenomenon. Expert Rev Cardiovasc Ther. 2007. 5:715–731.4. Ishihara M, Sato H, Tateishi H, Kawagoe T, Muraoka Y, Yoshimura M. Effects of intraaortic balloon pumping on coronary hemodynamics after coronary angioplasty in patients with acute myocardial infarction. Am Heart J. 1992. 124:1133–1138.5. Kurusz M, Zwischenberger JB. Percutaneous cardiopulmonary bypass for cardiac emergencies. Perfusion. 2002. 17:269–277.
Article6. Gibson CM, Jennings LK, Murphy SA, Lorenz DP, Giugliano RP, Harrington RA, et al. Association between platelet receptor occupancy after eptifibatide (integrilin) therapy and patency, myocardial perfusion, and ST-segment resolution among patients with ST-segment-elevation myocardial infarction: an INTEGRITI (Integrilin and Tenecteplase in Acute Myocardial Infarction) substudy. Circulation. 2004. 110:679–684.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Cardiopulmonary Bypass Support in a Patient with Acute Myocardial Infarction by Stent Thrombosis Complicated with Ventricular Tachycardia
- No-Reflow Phoenomenon by Intracoronary Thrombus in Acute Myocardial Infarction
- Acute Profound Thrombocytopenia after Using Abciximab for No-Reflow during Primary Percutaneous Coronary Intervention for ST-Segment Elevation Myocardial Infarction
- Effect of Percutaneous Transluminal Coronary Angioplasty in Treatment of Cardiogenic Shock Complicating Acute Myocardial Infarction
- Intraaortic Balloon Counterpulsation Support in Cardiogenic Shock due to Ventricular Septal Perforation and Huge Inferior Myocardial Infarction