Cancer Res Treat.
2012 Dec;44(4):227-234.
Definitive Radiotherapy versus Postoperative Radiotherapy for Tonsil Cancer
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. wuhg@snu.ac.kr
- 2Cancer Research Institution, Seoul National University College of Medicine, Seoul, Korea.
- 3Institution of Radiation Medicine, Medical Research Center, Seoul National University, Seoul, Korea.
- 4Department of Otorhinolaryngology and Head and Neck Surgery, Seoul National University, College of Medicine, Seoul, Korea.
- 5Department of Internal Medicine, Seoul National University, College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
The purpose of this study is to analyze treatment outcome of radiotherapy (RT) in patients with stage III-IV tonsil cancer managed by surgery followed by postoperative RT (SRT) and definitive chemoradiotherapy (CRT), and to thereby evaluate the most feasible treatment modality.
MATERIALS AND METHODS
Of 124 patients, 67 underwent CRT, and 57 underwent SRT. We compared survival and complication rates in both groups.
RESULTS
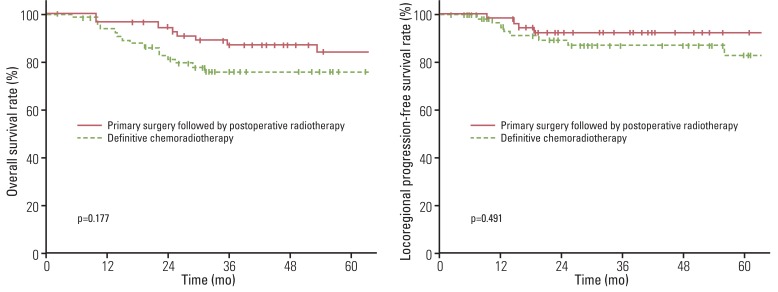
The median follow-up time was 57 months (range, 19 to 255 months) for surviving patients. At five years, locoregional progression-free survival (LRPFS) and overall survival (OS) were 88% and 80%, respectively. No significant difference in LRPFS (p=0.491) and OS (p=0.177) was observed between CRT and SRT. In multivariate analysis, old age and higher T stage showed a significant association with poor LRPFS, PFS, and OS; higher N stage showed an association with poor PFS and a trend of poor LRPFS, while no association with OS was observed; treatment modality (CRT and SRT) showed no association with LRFPS, PFS, and OS. Grade 3 or higher mucositis was observed in 12 patients (21%) in the SRT group, and 25 patients (37%) in the CRT group.
CONCLUSION
Definitive CRT and SRT have similar treatment outcomes for patients with stage III-IV tonsil cancer. Although acute complication rate appears to be higher in the CRT group, it should be noted that not all data on complications were included in this retrospective study. To determine the most feasible treatment modality, not only mucositis and xerostomia, but also emotional aspect and quality of life, should be considered.
MeSH Terms
Figure
Reference
-
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90. PMID: 21296855.
Article2. Kramer S, Gelber RD, Snow JB, Marcial VA, Lowry LD, Davis LW, et al. Combined radiation therapy and surgery in the management of advanced head and neck cancer: final report of study 73-03 of the Radiation Therapy Oncology Group. Head Neck Surg. 1987; 10:19–30. PMID: 3449477.
Article3. Shirazi HA, Sivanandan R, Goode R, Fee WE, Kaplan MJ, Pinto HA, et al. Advanced-staged tonsillar squamous carcinoma: organ preservation versus surgical management of the primary site. Head Neck. 2006; 28:587–594. PMID: 16475199.
Article4. Chang AR, Wu HG, Park CI, Kim KH, Sung MW, Heo DS. Retrospective analysis of the treatment results for patients with squamous cell carcinoma of tonsil. Cancer Res Treat. 2005; 37:92–97. PMID: 19956486.
Article5. Mendenhall WM, Amdur RJ, Stringer SP, Villaret DB, Cassisi NJ. Radiation therapy for squamous cell carcinoma of the tonsillar region: a preferred alternative to surgery? J Clin Oncol. 2000; 18:2219–2225. PMID: 10829041.
Article6. Mendenhall WM, Morris CG, Amdur RJ, Hinerman RW, Malyapa RS, Werning JW, et al. Definitive radiotherapy for tonsillar squamous cell carcinoma. Am J Clin Oncol. 2006; 29:290–297. PMID: 16755183.
Article7. Huang K, Xia P, Chuang C, Weinberg V, Glastonbury CM, Eisele DW, et al. Intensity-modulated chemoradiation for treatment of stage III and IV oropharyngeal carcinoma: the University of California-San Francisco experience. Cancer. 2008; 113:497–507. PMID: 18521908.8. de Arruda FF, Puri DR, Zhung J, Narayana A, Wolden S, Hunt M, et al. Intensity-modulated radiation therapy for the treatment of oropharyngeal carcinoma: the Memorial Sloan-Kettering Cancer Center experience. Int J Radiat Oncol Biol Phys. 2006; 64:363–373. PMID: 15925451.
Article9. Poulsen M, Porceddu SV, Kingsley PA, Tripcony L, Coman W. Locally advanced tonsillar squamous cell carcinoma: treatment approach revisited. Laryngoscope. 2007; 117:45–50. PMID: 17202929.
Article10. Pignon JP, le Maitre A, Maillard E, Bourhis J. MACH-NC Collaborative Group. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17,346 patients. Radiother Oncol. 2009; 92:4–14. PMID: 19446902.
Article11. Adelstein DJ, Lavertu P, Saxton JP, Secic M, Wood BG, Wanamaker JR, et al. Mature results of a phase III randomized trial comparing concurrent chemoradiotherapy with radiation therapy alone in patients with stage III and IV squamous cell carcinoma of the head and neck. Cancer. 2000; 88:876–883. PMID: 10679658.
Article12. Calais G, Alfonsi M, Bardet E, Sire C, Germain T, Bergerot P, et al. Randomized trial of radiation therapy versus concomitant chemotherapy and radiation therapy for advanced-stage oropharynx carcinoma. J Natl Cancer Inst. 1999; 91:2081–2086. PMID: 10601378.
Article13. Bonner JA, Harari PM, Giralt J, Cohen RB, Jones CU, Sur RK, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010; 11:21–28. PMID: 19897418.
Article14. Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB, et al. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med. 2006; 354:567–578. PMID: 16467544.
Article15. Chao KS, Ozyigit G, Tran BN, Cengiz M, Dempsey JF, Low DA. Patterns of failure in patients receiving definitive and postoperative IMRT for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2003; 55:312–321. PMID: 12527043.
Article16. Mittal BB, Pauloski BR, Haraf DJ, Pelzer HJ, Argiris A, Vokes EE, et al. Swallowing dysfunction: preventative and rehabilitation strategies in patients with head-and-neck cancers treated with surgery, radiotherapy, and chemotherapy: a critical review. Int J Radiat Oncol Biol Phys. 2003; 57:1219–1230. PMID: 14630255.17. Eisbruch A, Schwartz M, Rasch C, Vineberg K, Damen E, Van As CJ, et al. Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys. 2004; 60:1425–1439. PMID: 15590174.
Article18. Parsons JT, Mendenhall WM, Stringer SP, Amdur RJ, Hinerman RW, Villaret DB, et al. Squamous cell carcinoma of the oropharynx: surgery, radiation therapy, or both. Cancer. 2002; 94:2967–2980. PMID: 12115386.19. Boscolo-Rizzo P, Stellin M, Fuson R, Marchiori C, Gava A, Da Mosto MC. Long-term quality of life after treatment for locally advanced oropharyngeal carcinoma: surgery and postoperative radiotherapy versus concurrent chemoradiation. Oral Oncol. 2009; 45:953–957. PMID: 19665919.
Article20. Moore EJ, Olsen KD, Kasperbauer JL. Transoral robotic surgery for oropharyngeal squamous cell carcinoma: a prospective study of feasibility and functional outcomes. Laryngoscope. 2009; 119:2156–2164. PMID: 19824067.
Article21. Koshy M, Paulino AC, Howell R, Schuster D, Halkar R, Davis LW. F-18 FDG PET-CT fusion in radiotherapy treatment planning for head and neck cancer. Head Neck. 2005; 27:494–502. PMID: 15772951.
Article22. Jansen JF, Schoder H, Lee NY, Stambuk HE, Wang Y, Fury MG, et al. Tumor metabolism and perfusion in head and neck squamous cell carcinoma: pretreatment multimodality imaging with 1H magnetic resonance spectroscopy, dynamic contrast-enhanced MRI, and [18F]FDG-PET. Int J Radiat Oncol Biol Phys. 2012; 82:299–307. PMID: 21236594.
Article