Allergy Asthma Immunol Res.
2011 Jul;3(3):194-198. 10.4168/aair.2011.3.3.194.
Vancomycin-Associated Spontaneous Cutaneous Adverse Drug Reactions
- Affiliations
-
- 1Ajou Regional Pharmacovigilance Center, Ajou University Hospital, Suwon, Korea. youngmin.ye@gmail.com
- 2Department of Allergy and Clinical Immunology, Ajou University School of Medicine, Suwon, Korea.
- 3Department of Infectious Disease, Ajou University School of Medicine, Suwon, Korea.
- KMID: 1803325
- DOI: http://doi.org/10.4168/aair.2011.3.3.194
Abstract
- PURPOSE
With the increase in vancomycin use, adverse drug reactions (ADRs) associated with vancomycin have been reported increasingly more often. However, the characteristics of cutaneous ADRs with and without systemic reactions (SRs) have not been described. This study investigated the characteristics of spontaneously reported and assessed ADRs associated with vancomycin by a pharmacovigilance center.
METHODS
ADRs (n=121) associated with vancomycin in 96 patients were collected from 2008 to 2009. Records from physician- and nurse-reported suspected cases of vancomycin ADRs, ADR type, latent period, and laboratory results were compared between cutaneous ADRs with and without SRs.
RESULTS
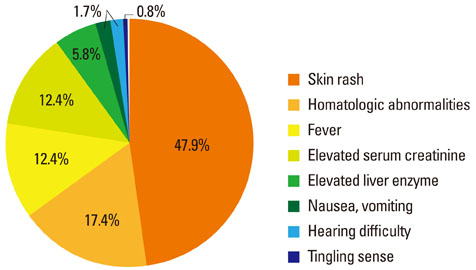
The main vancomycin-related ADRs were skin rashes (47.9%), hematologic abnormalities (17.36%), fever (12.4%), and elevated serum creatinine (12.4%). Significant differences were observed in latent period (days) and the mean change in eosinophils (%) between cutaneous (9.21+/-9.71 and 1.4+/-3.4, respectively) and other ADRs (14.03+/-11.71 and -0.5+/-3.5, respectively). Twelve cases of cutaneous ADRs with SRs had been initially reported as cutaneous ADRs only. Mean changes in the eosinophil count were significantly higher for cutaneous ADRs with SRs compared to those without SRs.
CONCLUSIONS
Skin rashes accompanied by peripheral eosinophilia, representing suspected immune-mediated delayed hypersensitivity reactions, are a common vancomycin ADR. For the early and exact detection of ADRs associated with vancomycin administration, close monitoring of laboratory tests, including complete blood counts with differential analysis, is recommended.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
T-cell lymphoma presenting as drug rash with eosinophilia and systemic symptoms syndrome
Mi-Ae Kim, Hye-Soo Yoo, Sun Hyuk Hwang, Yoo Seob Shin, Dong-Ho Nahm, Hae-Sim Park
Allergy Asthma Respir Dis. 2013;1(3):280-283. doi: 10.4168/aard.2013.1.3.280.Antibiotic-Induced Increase in Inflammatory Markers in Cured Infectious Spondylitis : Two Case Reports
Ki Seong Eom
J Korean Neurosurg Soc. 2019;62(4):487-491. doi: 10.3340/jkns.2018.0052.
Reference
-
1. Wong JT, Ripple RE, MacLean JA, Marks DR, Bloch KJ. Vancomycin hypersensitivity: synergism with narcotics and "desensitization" by a rapid continuous intravenous protocol. J Allergy Clin Immunol. 1994. 94:189–194.2. Sivagnanam S, Deleu D. Red man syndrome. Crit Care. 2003. 7:119–120.3. Levine DP. Vancomycin: a history. Clin Infect Dis. 2006. 42:Suppl 1. S5–S12.4. Kupstaite R, Baranauskaite A, Pileckyte M, Sveikata A, Kadusevicius E, Muckiene G. Severe vancomycin-induced anaphylactic reaction. Medicina (Kaunas). 2010. 46:30–33.5. Rocha JL, Kondo W, Baptista MI, Da Cunha CA, Martins LT. Uncommon vancomycin-induced side effects. Braz J Infect Dis. 2002. 6:196–200.6. Shah RA, Musthaq A, Khardori N. Vancomycin-induced thrombocytopenia in a 60-year-old man: a case report. J Med Case Reports. 2009. 3:7290.7. Kwon HS, Chang YS, Jeong YY, Lee SM, Song WJ, Kim HB, Kim YK, Cho SH, Kim YY, Min KU. A case of hypersensitivity syndrome to both vancomycin and teicoplanin. J Korean Med Sci. 2006. 21:1108–1110.8. Shin YS, Lee YW, Choi YH, Park B, Jee YK, Choi SK, Kim EG, Park JW, Hong CS. Spontaneous reporting of adverse drug events by Korean regional pharmacovigilance centers. Pharmacoepidemiol Drug Saf. 2009. 18:910–915.9. Kohno S, Yamaguchi K, Aikawa N, Sumiyama Y, Odagiri S, Aoki N, Niki Y, Watanabe S, Furue M, Ito T, Croos-Dabrera R, Tack KJ. Linezolid versus vancomycin for the treatment of infections caused by methicillin-resistant Staphylococcus aureus in Japan. J Antimicrob Chemother. 2007. 60:1361–1369.10. Wood MJ. Comparative safety of teicoplanin and vancomycin. J Chemother. 2000. 12:Suppl 5. 21–25.11. Thong BY. Update on the management of antibiotic allergy. Allergy Asthma Immunol Res. 2010. 2:77–86.12. Wallace MR, Mascola JR, Oldfield EC 3rd. Red man syndrome: incidence, etiology, and prophylaxis. J Infect Dis. 1991. 164:1180–1185.13. Polk RE, Healy DP, Schwartz LB, Rock DT, Garson ML, Roller K. Vancomycin and the red-man syndrome: pharmacodynamics of histamine release. J Infect Dis. 1988. 157:502–507.14. O'Sullivan TL, Ruffing MJ, Lamp KC, Warbasse LH, Rybak MJ. Prospective evaluation of red man syndrome in patients receiving vancomycin. J Infect Dis. 1993. 168:773–776.15. Levy JH, Kettlekamp N, Goertz P, Hermens J, Hirshman CA. Histamine release by vancomycin: a mechanism for hypotension in man. Anesthesiology. 1987. 67:122–125.16. Zuliani E, Zwahlen H, Gilliet F, Marone C. Vancomycin-induced hypersensitivity reaction with acute renal failure: resolution following cyclosporine treatment. Clin Nephrol. 2005. 64:155–158.17. Tamagawa-Mineoka R, Katoh N, Nara T, Nishimura Y, Yamamoto S, Kishimoto S. DRESS syndrome caused by teicoplanin and vancomycin, associated with reactivation of human herpesvirus-6. Int J Dermatol. 2007. 46:654–655.18. Yazganoglu KD, Ozkaya E, Ergin-Ozcan P, Cakar N. Vancomycin-induced drug hypersensitivity syndrome. J Eur Acad Dermatol Venereol. 2005. 19:648–650.19. Vauthey L, Uçkay I, Abrassart S, Bernard L, Assal M, Ferry T, Djordjevic M, Roussos C, Vaudaux P. Vancomycin-induced DRESS syndrome in a female patient. Pharmacology. 2008. 82:138–141.20. Polk RE, Israel D, Wang J, Venitz J, Miller J, Stotka J. Vancomycin skin tests and prediction of "red man syndrome" in healthy volunteers. Antimicrob Agents Chemother. 1993. 37:2139–2143.21. Perrin-Lamarre A, Petitpain N, Trechot P, Cuny JF, Schmutz JL, Barbaud A. Glycopeptide-induced cutaneous adverse reaction: results of an immunoallergic investigation in eight patients. Ann Dermatol Venereol. 2010. 137:101–105.22. Rosow CE, Moss J, Philbin DM, Savarese JJ. Histamine release during morphine and fentanyl anesthesia. Anesthesiology. 1982. 56:93–96.23. Moss J, Rosow CE. Histamine release by narcotics and muscle relaxants in humans. Anesthesiology. 1983. 59:330–339.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cutaneous adverse drug reactions
- Analysis of vancomycin-associated adverse reactions using a common data model
- Analysis of Drugs Causing Severe Cutaneous Adverse Reactions, Based on the Korean Database of Spontaneously Reported Adverse Drug Reactions
- Fentanyl PCA Monotherapy and Fentanyl TTS Combination Therapy in Post-Operative Pain Management: Analyses of Spontaneous Adverse Drug Reaction Reports
- Incidence of teicoplanin adverse drug reactions among patients with vancomycin-associated adverse drug reactions and its risk factors