Korean J Hepatobiliary Pancreat Surg.
2014 Aug;18(3):84-89. 10.14701/kjhbps.2014.18.3.84.
Clinical feasibility and nutritional effects of early oral feeding after pancreaticoduodenectomy
- Affiliations
-
- 1Department of Surgery, Daejeon Sun Hospital, Daejeon, Korea.
- 2Department of Nutrition Service, Chonbuk National University Hospital, Jeonju, Korea.
- 3Department of Surgery, Chonbuk National University Hospital, Chonbuk National University Medical School, and Research Institute of Clinical Medicine, Jeonju, Korea. hcyu@jbnu.ac.kr
- KMID: 1802219
- DOI: http://doi.org/10.14701/kjhbps.2014.18.3.84
Abstract
- BACKGROUNDS/AIMS
Pancreaticoduodenctomy (PD) is associated with high rates of postoperative morbidity and mortality. Although many studies have shown that early postoperative enteral nutrition improves postoperative outcomes, limited clinical information is available on postoperative early oral feeding (EOF) after PD. The aim of this study was to evaluate the clinical feasibility, safety, and nutritional effects of EOF after PD.
METHODS
Clinical outcomes were investigated in 131 patients who underwent PD between 2003 and 2013, including 81 whose oral feeding was commenced within 48 hours (EOF group) and 50 whose oral feeding was commenced after resumption of bowel movements (traditional oral feeding [TOF] group). Postoperative complications, energy intake, and length of stay (LOS) were reviewed.
RESULTS
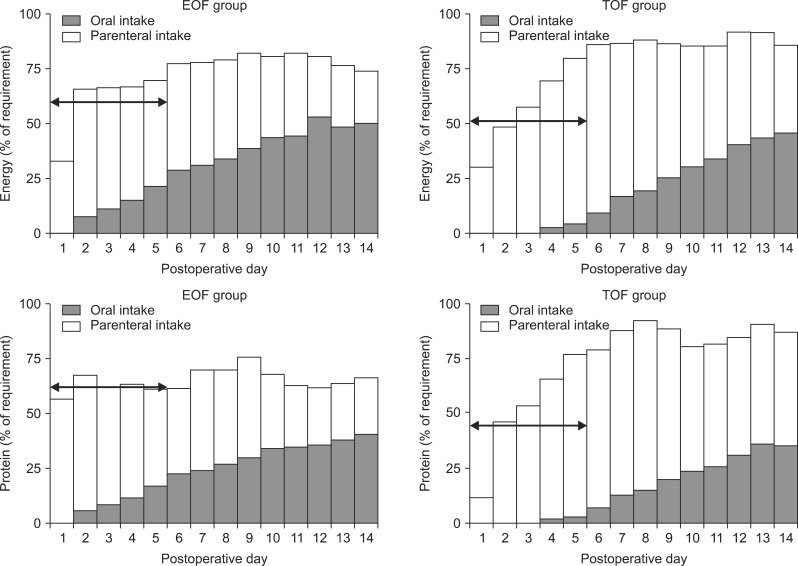
Demographic factors were similar in the two groups. The EOF group had a significantly shorter LOS (25.9+/-8.5 days vs. 32.3+/-16.3 days; p=0.01) than the TOF group. The rates of anastomotic leak (1.2% vs. 16%, p=0.00) and reoperation (3.7% vs. 20%, p=0.01) were significantly lower in the EOF group. In the clinically acute phase from postoperative day 1 to day 5, the mean daily calorie intake (847.0 kcal vs. 745.6 kcal; p=0.04) and mean daily protein intake (42.2 g vs. 31.9 g; p=0.00) in the EOF group were significantly higher than that in the TOF group.
CONCLUSIONS
Postoperative EOF is a clinically safe, feasible, and effective method of nutritional support after PD.
MeSH Terms
Figure
Cited by 2 articles
-
Effect of early and delay starting of enteral feeding in post-pancreaticoduodenectomy patients
Bidhan C. Das, Mozammel Haque, Mohammad Saief Uddin, Md. Nur-E-Elahi, Zulfiqur Rahman Khan
Ann Hepatobiliary Pancreat Surg. 2019;23(1):56-60. doi: 10.14701/ahbps.2019.23.1.56.A Study on the Dietary Intake and the Nutritional Status among the Pancreatic Cancer Surgical Patients
Jimin Kang, Joon Seong Park, Dong Sup Yoon, Woo Jeong Kim, Hae-yun Chung, Song Mi Lee, Namsoo Chang
Clin Nutr Res. 2016;5(4):279-289. doi: 10.7762/cnr.2016.5.4.279.
Reference
-
1. Gooiker GA, van Gijn W, Wouters MW, Post PN, van de Velde CJ, Tollenaar RA. Signalling Committee Cancer of the Dutch Cancer Society. Systematic review and meta-analysis of the volume-outcome relationship in pancreatic surgery. Br J Surg. 2011; 98:485–494. PMID: 21500187.
Article2. Okabayashi T, Kobayashi M, Nishimori I, Sugimoto T, Akimori T, Namikawa T, et al. Benefits of early postoperative jejunal feeding in patients undergoing duodenohemipancreatectomy. World J Gastroenterol. 2006; 12:89–93. PMID: 16440423.
Article3. Akbarshahi H, Andersson B, Nordén M, Andersson R. Perioperative nutrition in elective gastrointestinal surgery--potential for improvement? Dig Surg. 2008; 25:165–174. PMID: 18515968.4. Lassen K, Kjaeve J, Fetveit T, Tranø G, Sigurdsson HK, Horn A, et al. Allowing normal food at will after major upper gastrointestinal surgery does not increase morbidity: a randomized multicenter trial. Ann Surg. 2008; 247:721–729. PMID: 18438106.5. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007; 142:761–768. PMID: 17981197.
Article6. Lewis SJ, Andersen HK, Thomas S. Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg. 2009; 13:569–575. PMID: 18629592.7. Schroeder D, Gillanders L, Mahr K, Hill GL. Effects of immediate postoperative enteral nutrition on body composition, muscle function, and wound healing. JPEN J Parenter Enteral Nutr. 1991; 15:376–383. PMID: 1910100.
Article8. Moore FA, Feliciano DV, Andrassy RJ, McArdle AH, Booth FV, Morgenstein-Wagner TB, et al. Early enteral feeding, compared with parenteral, reduces postoperative septic complications. The results of a meta-analysis. Ann Surg. 1992; 216:172–183. PMID: 1386982.
Article9. Brennan MF, Pisters PW, Posner M, Quesada O, Shike M. A prospective randomized trial of total parenteral nutrition after major pancreatic resection for malignancy. Ann Surg. 1994; 220:436–441. PMID: 7944656.
Article10. Nagata S, Fukuzawa K, Iwashita Y, Kabashima A, Kinoshita T, Wakasugi K, et al. Comparison of enteral nutrition with combined enteral and parenteral nutrition in post-pancreaticoduodenectomy patients: a pilot study. Nutr J. 2009; 8:24. PMID: 19519910.
Article11. Wayne MG, Jorge IA, Cooperman AM. Alternative reconstruction after pancreaticoduodenectomy. World J Surg Oncol. 2008; 6:9. PMID: 18221566.
Article12. Alexander JW. Bacterial translocation during enteral and parenteral nutrition. Proc Nutr Soc. 1998; 57:389–393. PMID: 9793995.
Article13. Fukuzawa J, Terashima H, Ohkohchi N. Early postoperative oral feeding accelerates upper gastrointestinal anastomotic healing in the rat model. World J Surg. 2007; 31:1234–1239. PMID: 17468901.
Article14. Nachlas MM, Younis MT, Roda CP, Wityk JJ. Gastrointestinal motility studies as a guide to postoperative management. Ann Surg. 1972; 175:510–522. PMID: 5020667.
Article15. Deitch EA, Winterton J, Li M, Berg R. The gut as a portal of entry for bacteremia. Role of protein malnutrition. Ann Surg. 1987; 205:681–692. PMID: 3592811.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Intervention for Developmental Delayed Children with Swallowing and Feeding Disorders
- Postoperative Nutritional Effects of Early Enteral Feeding Compared with Total Parental Nutrition in Pancreaticoduodectomy Patients: A Prosepective, Randomized Study
- Nutritional Considerations in Tube Feeding Patients
- Evaluation and Treatment of Malnutrition and Associated Gastrointestinal Complications in Children with Cerebral Palsy
- Surgical feeding tube insertion, the literature review and the actual procedure