Ann Surg Treat Res.
2015 Jun;88(6):311-317. 10.4174/astr.2015.88.6.311.
Analysis of patient-dropouts from the critical pathways for gastric cancer
- Affiliations
-
- 1Department of Surgery, Chosun University College of Medicine, Gwangju, Korea. ysyoo@chosun.ac.kr
- 2Department of Nursing Science, Chosun University, Gwangju, Korea.
- KMID: 1800644
- DOI: http://doi.org/10.4174/astr.2015.88.6.311
Abstract
- PURPOSE
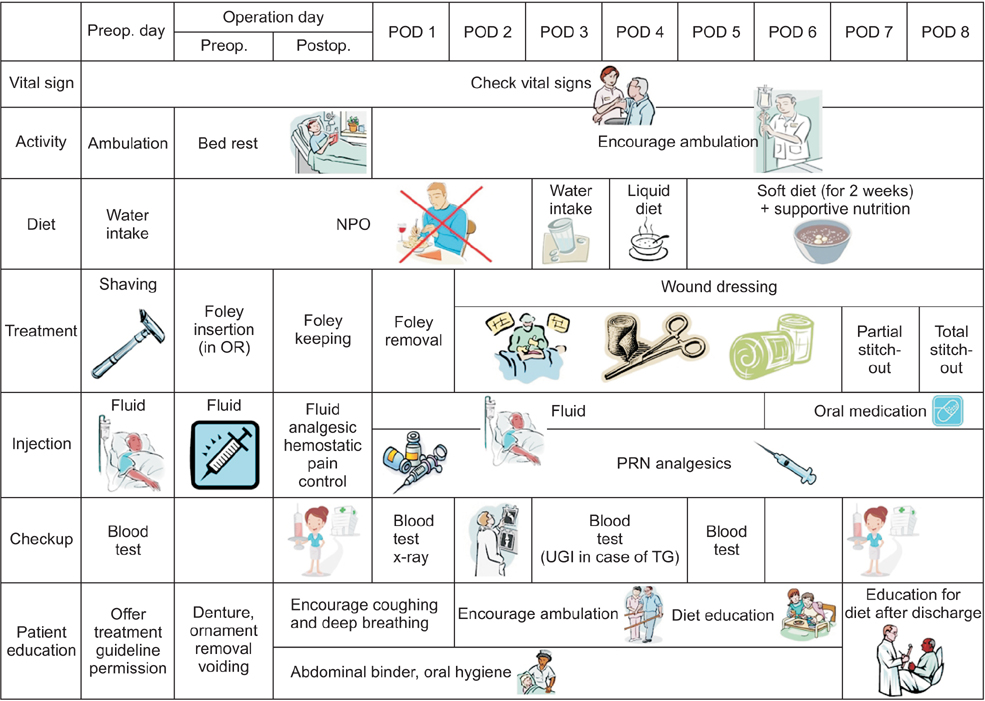
This study was designed to determine the factors affecting completion of critical pathway for elective gastrectomy.
METHODS
Since 2008, a critical pathway has been applied for elective gastrectomy at Chosun University Hospital. We retrospectively analyzed 252 patients who underwent elective gastrectomies from January 2009 to April 2013. The completion rate was determined, and risk factors for patient dropout were examined.
RESULTS
The completion rate of the critical pathway was 45.6% (115/252). Mean length of stay was 11.7 +/- 8.6 days (8-59 days). Readmission rates were 4.4% (11/252). Causes of failure for clinical pathway were systemic complications (21/137, 15.3%), intra-abdominal complications (44/137, 32.8%), patient factors (41/137, 29.9%), and wound complications (30/137, 21.9%). There were no significant differences between the two groups in age, sex, American Society of Anesthesiologists (ASA) score, operation time, readmission, and underlying disease (P > 0.05). Body mass index (P = 0.008) and pathologic stage (P = 0.001) were significantly different between the two groups. In multivariate analysis, the conventional approach (odds ratio, 2.0), and total gastrectomy (odds ratio, 5.3) were determined to be independent risk factors to drop the critical pathway. But there were no significant differences between total and distal gastrectomy groups in age, gender, underlying diseases, ASA score, readmission, operation time, and cause of dropout (P > 0.05).
CONCLUSION
We concluded that total gastrectomy may not be suitable for the critical pathway. We suggest that the critical pathway for elective distal gastrectomy is divided 2 subgroups, according to the surgical approach.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Reduction rate of C-reactive protein as an early predictor of postoperative complications and a reliable discharge indicator after gastrectomy for gastric cancer
Si-Hak Lee, Ki Hyun Kim, Cheol Woong Choi, Su Jin Kim, Dae-Hwan Kim, Chang In Choi, Sun-Hwi Hwang
Ann Surg Treat Res. 2019;97(2):65-73. doi: 10.4174/astr.2019.97.2.65.
Reference
-
1. Rotter T, Kinsman L, James E, Machotta A, Willis J, Snow P, et al. The effects of clinical pathways on professional practice, patient outcomes, length of stay, and hospital costs: Cochrane systematic review and meta-analysis. Eval Health Prof. 2012; 35:3–27.2. Zhang M, Zhou SY, Xing MY, Xu J, Shi XX, Zheng SS. The application of clinical pathways in laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int. 2014; 13:348–353.3. Saint S, Hofer TP, Rose JS, Kaufman SR, McMahon LF Jr. Use of critical pathways to improve efficiency: a cautionary tale. Am J Manag Care. 2003; 9:758–765.4. Nussbaum DP, Penne K, Stinnett SS, Speicher PJ, Cocieru A, Blazer DG 3rd, et al. A standardized care plan is associated with shorter hospital length of stay in patients undergoing pancreaticoduodenectomy. J Surg Res. 2015; 193:237–245.5. Seo HS, Song KY, Jeon HM, Park CH. The impact of an increased application of critical pathway for gastrectomy on the length of stay and cost. J Gastric Cancer. 2012; 12:126–131.6. Jeong SH, Yoo MW, Yoon HM, Lee HJ, Ahn HS, Cho JJ, et al. Is the critical pathway effective for the treatment of gastric cancer? J Korean Surg Soc. 2011; 81:96–103.7. Choi JW, Xuan Y, Hur H, Byun CS, Han SU, Cho YK. Outcomes of critical pathway in laparoscopic and open surgical treatments for gastric cancer patients: patients selection for fast-track program through retrospective analysis. J Gastric Cancer. 2013; 13:98–105.8. Walters DM, McGarey P, LaPar DJ, Strong A, Good E, Adams RB, et al. A 6-day clinical pathway after a pancreaticoduodenectomy is feasible, safe and efficient. HPB (Oxford). 2013; 15:668–673.9. Pearson SD, Goulart-Fisher D, Lee TH. Critical pathways as a strategy for improving care: problems and potential. Ann Intern Med. 1995; 123:941–948.10. Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009; 361:1368–1375.11. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009; 360:1418–1428.12. Lee KG, Lee HJ, Yang JY, Oh SY, Bard S, Suh YS, et al. Risk factors associated with complication following gastrectomy for gastric cancer: retrospective analysis of prospectively collected data based on the Clavien-Dindo system. J Gastrointest Surg. 2014; 18:1269–1277.13. Bartlett EK, Roses RE, Kelz RR, Drebin JA, Fraker DL, Karakousis GC. Morbidity and mortality after total gastrectomy for gastric malignancy using the American College of Surgeons National Surgical Quality Improvement Program database. Surgery. 2014; 156:298–304.14. Cheng Q, Pang TC, Hollands MJ, Richardson AJ, Pleass H, Johnston ES, et al. Systematic review and meta-analysis of laparoscopic versus open distal gastrectomy. J Gastrointest Surg. 2014; 18:1087–1099.15. Li HT, Han XP, Su L, Zhu WK, Xu W, Li K, et al. Short-term efficacy of laparoscopyassisted vs open radical gastrectomy in gastric cancer. World J Gastrointest Surg. 2014; 6:59–64.16. Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008; 248:721–727.17. Viñuela EF, Gonen M, Brennan MF, Coit DG, Strong VE. Laparoscopic versus open distal gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized studies. Ann Surg. 2012; 255:446–456.18. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995; 854:1–452.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes of Critical Pathway in Laparoscopic and Open Surgical Treatments for Gastric Cancer Patients: Patients Selection for Fast-Track Program through Retrospective Analysis
- Critical Pathway for Operable Gastric Cancer
- Critical Pathways for Cesarean Section
- Molecular Diagnosis for Personalized Target Therapy in Gastric Cancer
- The Impact of an Increased Application of Critical Pathway for Gastrectomy on the Length of Stay and Cost