Imaging Sci Dent.
2014 Jun;44(2):165-169. 10.5624/isd.2014.44.2.165.
Clival lesion incidentally discovered on cone-beam computed tomography: A case report and review of the literature
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology, University of Connecticut School of Dental Medicine, Farmington, CT, USA. dr.aniket.jadhav@gmail.com
- 2Division of Diagnostic Sciences and Therapeutics, University of Connecticut School of Medicine, Farmington, CT, USA.
- KMID: 1799600
- DOI: http://doi.org/10.5624/isd.2014.44.2.165
Abstract
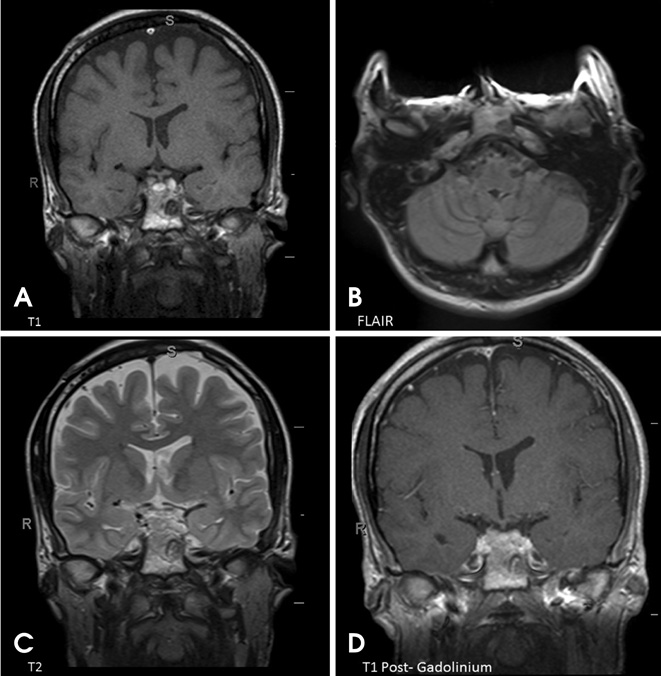
- An osteolytic lesion with a small central area of mineralization and sclerotic borders was discovered incidentally in the clivus on the cone-beam computed tomography (CBCT) of a 27-year-old male patient. This benign appearance indicated a primary differential diagnosis of non-aggressive lesions such as fibro-osseous lesions and arrested pneumatization. Further, on magnetic resonance imaging (MRI), the lesion showed a homogenously low T1 signal intensity with mild internal enhancement after post-gadolinium and a heterogeneous T2 signal intensity. These signal characteristics might be attributed to the fibrous tissues, chondroid matrix, calcific material, or cystic component of the lesion; thus, chondroblastoma and chondromyxoid fibroma were added to the differential diagnosis. Although this report was limited by the lack of final diagnosis and the patient lost to follow-up, the incidental skull base finding would be important for interpreting the entire volume of CBCT by a qualified oral and maxillofacial radiologist.
Keyword
MeSH Terms
Figure
Reference
-
1. Alhadidi A, Cevidanes LH, Paniagua B, Cook R, Festy F, Tyndall D. 3D quantification of mandibular asymmetry using the SPHARM-PDM tool box. Int J Comput Assist Radiol Surg. 2012; 7:265–271.
Article2. Swennen GR, Mollemans W, Schutyser F. Three-dimensional treatment planning of orthognathic surgery in the era of virtual imaging. J Oral Maxillofac Surg. 2009; 67:2080–2092.
Article3. Price JB, Thaw KL, Tyndall DA, Ludlow JB, Padilla RJ. Incidental findings from cone beam computed tomography of the maxillofacial region: a descriptive retrospective study. Clin Oral Implants Res. 2012; 23:1261–1268.
Article4. Laine FJ, Nadel L, Braun IF. CT and MR imaging of the central skull base. Part 1: Techniques, embryologic development, and anatomy. Radiographics. 1990; 10:591–602.
Article5. Chaljub G, Van Fleet R, Guinto FC Jr, Crow WN, Martinez L, Kumar R. MR imaging of clival and paraclival lesions. AJR Am J Roentgenol. 1992; 159:1069–1074.
Article6. Welker KM, DeLone DR, Lane JI, Gilbertson JR. Arrested pneumatization of the skull base: imaging characteristic. AJR Am J Roentgenol. 2008; 190:1691–1696.7. Bloch OG, Jian BJ, Yang I, Han SJ, Aranda D, Ahn BJ, et al. Cranial chondrosarcoma and recurrence. Skull Base. 2010; 20:149–156.
Article8. Borges A. Skull base tumours: Part II. Central skull base tumours and intrinsic tumours of the bony skull base. Eur J Radiol. 2008; 66:348–362.9. Douis H, Saifuddin A. The imaging of cartilaginous bone tumours. II. Chondrosarcoma. Skeletal Radiol. 2013; 42:611–626.
Article10. Géhanne C, Delpierre I, Damry N, Devroede B, Brihaye P, Christophe C. Skull base chordoma: CT and MRI features. JBR-BTR. 2005; 88:325–327.11. Wein RO, Popat SR, Doerr TD, Dutcher PO. Plasma cell tumors of the skull base: four case reports and literature review. Skull Base. 2002; 12:77–86.
Article12. Borges A. Imaging of the central skull base. Neuroimaging Clin N Am. 2009; 19:669–696.
Article13. Ben Salem D, Allaoui M, Dumousset E, Ponnelle T, Justrabo E, Martin D, et al. Chondroblastoma of the temporal bone associated with a persistent hypoglossal artery. Acta Neurochir (Wien). 2002; 144:1315–1318.14. Hatano M, De Donato G, Falcioni M, Sanna M. Chondroblastoma of the temporal bone. Acta Otolaryngol. 2011; 131:890–895.
Article15. Dran G, Niesar E, Vandenbos F, Noel G, Paquis P, Lonjon M. Chondroblastoma of the apex portion of petrousal bone. Childs Nerv Syst. 2007; 23:231–235.
Article16. Weber AL. Imaging of the skull base. Eur J Radiol. 1996; 22:68–81.
Article17. Scarfe WC, Li Z, Aboelmaaty W, Scott SA, Farman AG. Maxillofacial cone beam computed tomography: essence, elements and steps to interpretation. Aust Dent J. 2012; 57:Suppl 1. 46–60.
Article18. Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol. 2010; 7:754–773.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Foramen transversarium enlargement caused by vertebral artery tortuosity: Diagnosis with cone-beam computed tomography and magnetic resonance angiography
- Detection of maxillary second molar with two palatal roots using cone beam computed tomography: a case report
- Cone beam computed tomography findings of ectopic mandibular third molar in the mandibular condyle: report of a case
- Isolated tympanic plate fracture detected by cone-beam computed tomography: report of four cases with review of literature
- Cone beam CT findings of retromolar canals: Report of cases and literature review