J Korean Med Sci.
2014 Jun;29(6):805-810. 10.3346/jkms.2014.29.6.805.
Efficacy of Hemocontrol Biofeedback System in Intradialytic Hypotension-Prone Hemodialysis Patients
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- 2Department of Internal Medicine, Eulji University School of Medicine, Daejeon, Korea.
- 3Department of Internal Medicine, Eulji University School of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 5Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 6Department of Internal Medicine, The Catholic University of Korea, Uijeongbu St. Mary's Hospital, Uijeongbu, Korea.
- 7Department of Internal Medicine, The Catholic University of Korea, Bucheon St. Mary's Hospital, Bucheon, Korea.
- 8Department of Internal Medicine, Korea University Guro Hospital, Seoul, Korea.
- 9Department of Internal Medicine, The Catholic University of Korea, Seoul St. Mary's Hospital, Seoul, Korea. kimcmc@catholic.ac.kr
- KMID: 1796943
- DOI: http://doi.org/10.3346/jkms.2014.29.6.805
Abstract
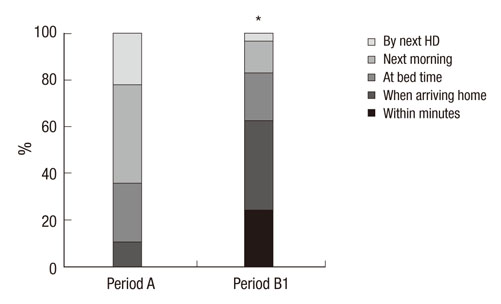
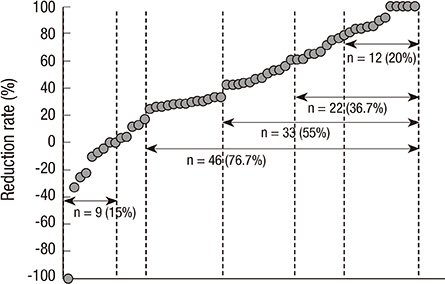
- We conducted a study to determine whether the hemocontrol biofeedback system (HBS) can improve intradialytic hypotension (IDH) in hypotension-prone hemodialysis (HD) patients compared with conventional HD. In this multicenter prospective crossover study, 60 hypotension-prone patients were serially treated by conventional HD for 8 weeks (period A), by HD with hemoscan blood volume monitoring for 2 weeks (period B0), and by HBS HD for 8 weeks (period B1). The number of sessions complicated by symptomatic IDH during 24 HD sessions (14.9+/-5.8 sessions, 62.1% in period A vs 9.2+/-7.2 sessions, 38.4% in period B1, P<0.001) and the number of IDH-related nursing interventions in a session (0.96+/-0.66 in period A vs 0.56+/-0.54 in period B1, P<0.001) significantly decreased in period B1 than in period A. Recovery time from fatigue after dialysis was significantly shorter in period B1 than in period A. The patients with higher post-dialysis blood pressure, lower difference between pre- and post-dialysis blood pressure, less frequent IDH, and higher pre- and post-dialysis body weight in period A responded better to HBS in period B1 in regard to the reduction of IDH. In conclusion, HBS may improve the patient tolerability to HD by reducing the IDH frequency and promoting faster recovery from fatigue after dialysis.
Keyword
MeSH Terms
Figure
Reference
-
1. Daugirdas JT. Pathophysiology of dialysis hypotension: an update. Am J Kidney Dis. 2001; 38:S11–S17.2. Sulowicz W, Radziszewski A. Pathogenesis and treatment of dialysis hypotension. Kidney Int. 2006; 70:S36–S39.3. Henderson LW. Symptomatic intradialytic hypotension and mortality: an opinionated review. Semin Dial. 2012; 25:320–325.4. Selby NM, Lambie SH, Camici PG, Baker CS, McIntyre CW. Occurrence of regional left ventricular dysfunction in patients undergoing standard and biofeedback dialysis. Am J Kidney Dis. 2006; 47:830–841.5. Shoji T, Tsubakihara Y, Fujii M, Imai E. Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients. Kidney Int. 2004; 66:1212–1220.6. Sherman RA. Intradialytic hypotension: an overview of recent, unresolved and overlooked issues. Semin Dial. 2002; 15:141–143.7. Agarwal R. How can we prevent intradialytic hypotension? Curr Opin Nephrol Hypertens. 2012; 21:593–599.8. Sherman RA, Torres F, Cody RP. Postprandial blood pressure changes during hemodialysis. Am J Kidney Dis. 1988; 12:37–39.9. Palmer BF, Henrich WL. Recent advances in the prevention and management of intradialytic hypotension. J Am Soc Nephrol. 2008; 19:8–11.10. Zhou YL, Liu HL, Duan XF, Yao Y, Sun Y, Liu Q. Impact of sodium and ultrafiltration profiling on haemodialysis-related hypotension. Nephrol Dial Transplant. 2006; 21:3231–3237.11. Van der Sande FM, Wystrychowski G, Kooman JP, Rosales L, Raimann J, Kotanko P, Carter M, Chan CT, Leunissen KM, Levin NW. Control of core temperature and blood pressure stability during hemodialysis. Clin J Am Soc Nephrol. 2009; 4:93–98.12. Gabutti L, Bianchi G, Soldini D, Marone C, Burnier M. Haemodynamic consequences of changing bicarbonate and calcium concentrations in haemodialysis fluids. Nephrol Dial Transplant. 2009; 24:973–981.13. Prakash S, Garg AX, Heidenheim AP, House AA. Midodrine appears to be safe and effective for dialysis-induced hypotension: a systematic review. Nephrol Dial Transplant. 2004; 19:2553–2558.14. Locatelli F, Altieri P, Andrulli S, Bolasco P, Sau G, Pedrini LA, Basile C, David S, Feriani M, Montagna G, et al. Hemofiltration and hemodiafiltration reduce intradialytic hypotension in ESRD. J Am Soc Nephrol. 2010; 21:1798–1807.15. Ronco C, Brendolan A, Milan M, Rodeghiero MP, Zanella M, La Greca G. Impact of biofeedback-induced cardiovascular stability on hemodialysis tolerance and efficiency. Kidney Int. 2000; 58:800–808.16. Basile C, Giordano R, Vernaglione L, Montanaro A, De Maio P, De Padova F, Marangi AL, Di Marco L, Santese D, Semeraro A, et al. Efficacy and safety of haemodialysis treatment with the Hemocontrol biofeedback system: a prospective medium-term study. Nephrol Dial Transplant. 2001; 16:328–334.17. Santoro A, Mancini E, Basile C, Amoroso L, Di Giulio S, Usberti M, Colasanti G, Verzetti G, Rocco A, Imbasciati E, et al. Blood volume controlled hemodialysis in hypotension-prone patients: a randomized, multicenter controlled trial. Kidney Int. 2002; 62:1034–1045.18. Reddan DN, Szczech LA, Hasselblad V, Lowrie EG, Lindsay RM, Himmelfarb J, Toto RD, Stivelman J, Winchester JF, Zillman LA, et al. Intradialytic blood volume monitoring in ambulatory hemodialysis patients: a randomized trial. J Am Soc Nephrol. 2005; 16:2162–2169.19. Déziel C, Bouchard J, Zellweger M, Madore F. Impact of hemocontrol on hypertension, nursing interventions, and quality of life: a randomized, controlled trial. Clin J Am Soc Nephrol. 2007; 2:661–668.20. Bégin V, Déziel C, Madore F. Biofeedback regulation of ultrafiltration and dialysate conductivity for the prevention of hypotension during hemodialysis. ASAIO J. 2002; 48:312–315.21. Franssen CF, Dasselaar JJ, Sytsma P, Burgerhof JG, de Jong PE, Huisman RM. Automatic feedback control of relative blood volume changes during hemodialysis improves blood pressure stability during and after dialysis. Hemodial Int. 2005; 9:383–392.22. McIntyre CW, Lambie SH, Fluck RJ. Biofeedback controlled hemodialysis (BF-HD) reduces symptoms and increases both hemodynamic tolerability and dialysis adequacy in non-hypotension prone stable patients. Clin Nephrol. 2003; 60:105–112.23. Nesrallah GE, Suri RS, Thiessen-Philbrook H, Heidenheim P, Lindsay RM. Can extracellular fluid volume expansion in hemodialysis patients be safely reduced using the hemocontrol biofeedback algorithm? a randomized trial. ASAIO J. 2008; 54:270–274.24. Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care. 2003; 26:1553–1579.25. Karayannis G, Giamouzis G, Cokkinos DV, Skoularigis J, Triposkiadis F. Diabetic cardiovascular autonomic neuropathy: clinical implications. Expert Rev Cardiovasc Ther. 2012; 10:747–765.26. Vita G, Bellinghieri G, Trusso A, Costantino G, Santoro D, Monteleone F, Messina C, Savica V. Uremic autonomic neuropathy studied by spectral analysis of heart rate. Kidney Int. 1999; 56:232–237.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- System of integrating biosignals during hemodialysis: the CONTINUAL (Continuous mOnitoriNg viTal sIgN dUring hemodiALysis) registry
- The Effect of Cool Dialysate & Sodium Profiling on Hemodynamics in Patients with Intradialytic Hypotension
- Impacts of Coronary Artery Calcification on Intradialytic Blood Pressure Patterns in Patients Receiving Maintenance Hemodialysis
- Use of fludrocortisone for intradialytic hypotension
- Elucidation of the pathophysiology of intradialytic muscle cramps: pharmacokinetics applied to translational research