Yonsei Med J.
2013 Sep;54(5):1194-1201. 10.3349/ymj.2013.54.5.1194.
Proteinuria as a Risk Factor for Mortality in Patients with Colorectal Cancer
- Affiliations
-
- 1Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea. skimw@chonnam.ac.kr
- 2Department of Preventive Medicine, Chonnam National University Medical School, Gwangju, Korea.
- 3Jeonnam Regional Cancer Center, Chonnam National University Hwasun Hospital, Hwasun, Korea.
- KMID: 1793167
- DOI: http://doi.org/10.3349/ymj.2013.54.5.1194
Abstract
- PURPOSE
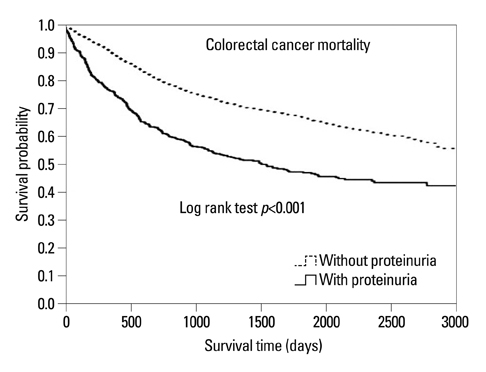
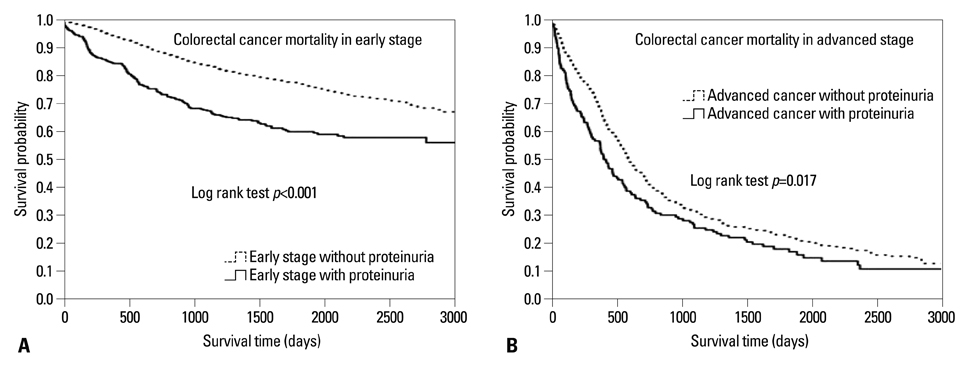
We investigated the effects of proteinuria and renal insufficiency on all-cause mortality in patients with colorectal cancer, with special emphasis on cancer staging and cancer-related deaths.
MATERIALS AND METHODS
We retrospectively studied a cohort of patients with colorectal cancer. In protocol 1, patients were classified into four groups based on the operability of cancer and proteinuria: group 1, early-stage cancer patients (colorectal cancer stage < or =3) without proteinuria; group 2, early-stage cancer patients with proteinuria; group 3, advanced-stage cancer patients without proteinuria (colorectal cancer stage=4); and group 4, advanced-stage cancer patients with proteinuria. In protocol 2, patients were classified into four similar groups based on cancer staging and renal insufficiency (eGFR <60 mL/min/1.73 m2). Between January 1, 1998 and December 31, 2009, 3379 patients were enrolled in this cohort and followed until May 1, 2012 or until death.
RESULTS
The number of patients with proteinuria was 495 (14.6%). The prevalence of proteinuria was higher in advanced-stage cancer (n=151, 22.3%) than in early-stage cancer patients (n=344, 12.7%). After adjusting for age, gender and other clinical variables, the proteinuric, early-stage cancer group was shown to be associated with an adjusted hazard ratio of 1.67 and a 95% confidence interval of 1.38-2.01, compared with non-proteinuric early-stage cancer patients. However, renal insufficiency was not associated with colorectal cancer mortality.
CONCLUSION
Proteinuria is an important risk factor for cancer mortality, especially in relatively early colorectal cancer.
Keyword
- Cancer; death; proteinuria; GFR; stage
MeSH Terms
Figure
Reference
-
1. Jung KW, Park S, Won YJ, Kong HJ, Lee JY, Seo HG, et al. Prediction of cancer incidence and mortality in Korea, 2012. Cancer Res Treat. 2012; 44:25–31.
Article2. Bufill JA. Colorectal cancer: evidence for distinct genetic categories based on proximal or distal tumor location. Ann Intern Med. 1990; 113:779–788.
Article3. Fried LF, Katz R, Sarnak MJ, Shlipak MG, Chaves PH, Jenny NS, et al. Kidney function as a predictor of noncardiovascular mortality. J Am Soc Nephrol. 2005; 16:3728–3735.
Article4. Roper NA, Bilous RW, Kelly WF, Unwin NC, Connolly VM. South Tees Diabetes Mortality Study. Cause-specific mortality in a population with diabetes: South Tees Diabetes Mortality Study. Diabetes Care. 2002; 25:43–48.5. Saydah SH, Loria CM, Eberhardt MS, Brancati FL. Abnormal glucose tolerance and the risk of cancer death in the United States. Am J Epidemiol. 2003; 157:1092–1100.
Article6. Weng PH, Hung KY, Huang HL, Chen JH, Sung PK, Huang KC. Cancer-specific mortality in chronic kidney disease: longitudinal follow-up of a large cohort. Clin J Am Soc Nephrol. 2011; 6:1121–1128.
Article7. Na SY, Sung JY, Chang JH, Kim S, Lee HH, Park YH, et al. Chronic kidney disease in cancer patients: an independent predictor of cancer-specific mortality. Am J Nephrol. 2011; 33:121–130.
Article8. Pedersen LM, Milman N. Microalbuminuria in patients with lung cancer. Eur J Cancer. 1998; 34:76–80.
Article9. Pedersen LM, Johnsen HE. Microalbuminuria is associated with impaired glomerular permselectivity in lymphoma patients. Scand J Clin Lab Invest. 2005; 65:477–484.
Article10. Pedersen LM, Sørensen PG. Mediators of inflammation correlate with microalbuminuria in patients with non-Hodgkin's lymphoma. Br J Haematol. 2003; 121:275–279.
Article11. Pedersen LM, Milman N. Prevalence and prognostic significance of proteinuria in patients with lung cancer. Acta Oncol. 1996; 35:691–695.
Article12. Pedersen LM, Sørensen PG. Increased urinary albumin excretion rate in breast cancer patients. Acta Oncol. 2000; 39:145–149.
Article13. Pedersen LM, Sørensen PG. Clinical significance of urinary albumin excretion in patients with non-Hodgkin's lymphoma. Br J Haematol. 1999; 107:889–891.
Article14. Pedersen LM, Sørensen PG. Urinary albumin excretion is a predictor of response to treatment and disease progression in low-grade non-Hodgkin's lymphoma. Leuk Lymphoma. 2004; 45:547–551.
Article15. Sawyer N, Wadsworth J, Wijnen M, Gabriel R. Prevalence, concentration, and prognostic importance of proteinuria in patients with malignancies. Br Med J (Clin Res Ed). 1988; 296:1295–1298.
Article16. Roumen RM, Wijnen MH. Proteinuria: a frequent paraneoplastic phenomenon in colorectal cancer? Eur J Cancer. 1998; 34:206–207.17. Puolijoki H, Mustonen J, Pettersson E, Pasternack A, Lahdensuo A. Proteinuria and haematuria are frequently present in patients with lung cancer. Nephrol Dial Transplant. 1989; 4:947–950.
Article18. Georgiannos SN, Weston PM, Goode AW. Correlation between albuminuria and positively charged amino acids in gastrointestinal cancer. Int Surg. 1995; 80:49–52.19. Vaglio A, Buzio L, Cravedi P, Pavone L, Garini G, Buzio C. Prognostic significance of albuminuria in patients with renal cell cancer. J Urol. 2003; 170(4 Pt 1):1135–1137.
Article20. Pedersen LM, Terslev L, SŁrensen PG, Stokholm KH. Urinary albumin excretion and transcapillary escape rate of albumin in malignancies. Med Oncol. 2000; 17:117–122.
Article21. Greene FL. Current TNM staging of colorectal cancer. Lancet Oncol. 2007; 8:572–573.
Article22. Engstrom PF, Arnoletti JP, Benson AB 3rd, Chen YJ, Choti MA, Cooper HS, et al. NCCN Clinical Practice Guidelines in Oncology: colon cancer. J Natl Compr Canc Netw. 2009; 7:778–831.23. Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006; 145:247–254.
Article24. Karalliedde J, Viberti G. Microalbuminuria and cardiovascular risk. Am J Hypertens. 2004; 17:986–993.
Article25. Lin YS, Chiu FC, Lin JW, Hwang JJ, Caffrey JL. Association of albuminuria and cancer mortality. Cancer Epidemiol Biomarkers Prev. 2010; 19:2950–2957.
Article26. Stehouwer CD, Gall MA, Twisk JW, Knudsen E, Emeis JJ, Parving HH. Increased urinary albumin excretion, endothelial dysfunction, and chronic low-grade inflammation in type 2 diabetes: progressive, interrelated, and independently associated with risk of death. Diabetes. 2002; 51:1157–1165.
Article27. Gorriz JL, Martinez-Castelao A. Proteinuria: detection and role in native renal disease progression. Transplant Rev (Orlando). 2012; 26:3–13.
Article28. Sutherland JC, Markham RV Jr, Mardiney MR Jr. Subclinical immune complexes in the glomeruli of kidneys postmortem. Am J Med. 1974; 57:536–541.
Article29. Pascal RR, Iannaccone PM, Rollwagen FM, Harding TA, Bennett SJ. Electron microscopy and immunofluorescence of glomerular immune complex deposits in cancer patients. Cancer Res. 1976; 36:43–47.30. Beaufils H, Jouanneau C, Chomette G. Kidney and cancer: results of immunofluorescence microscopy. Nephron. 1985; 40:303–308.
Article31. Wu MT, Lam KK, Lee WC, Hsu KT, Wu CH, Cheng BC, et al. Albuminuria, proteinuria, and urinary albumin to protein ratio in chronic kidney disease. J Clin Lab Anal. 2012; 26:82–92.
Article