J Korean Med Sci.
2010 Dec;25(12):1742-1747. 10.3346/jkms.2010.25.12.1742.
A Long Term Results of External Beam Radiation Therapy in Hemophilic Arthropathy of the Ankle in Children
- Affiliations
-
- 1Department of Radiation Oncology, Kyung Hee University School of Medicine, Seoul, Korea. kangjino@paran.com
- KMID: 1792897
- DOI: http://doi.org/10.3346/jkms.2010.25.12.1742
Abstract
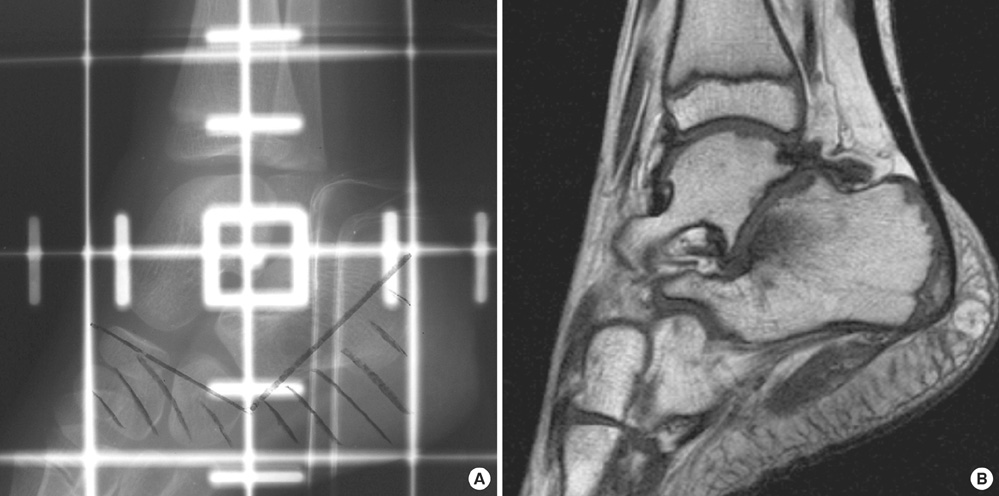
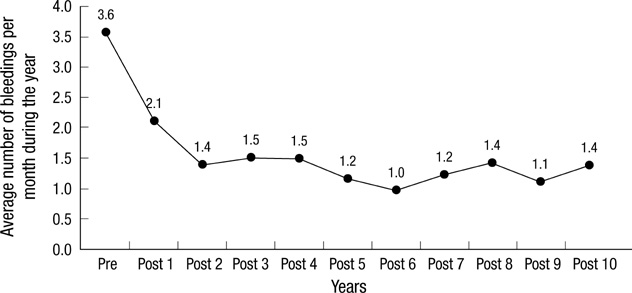
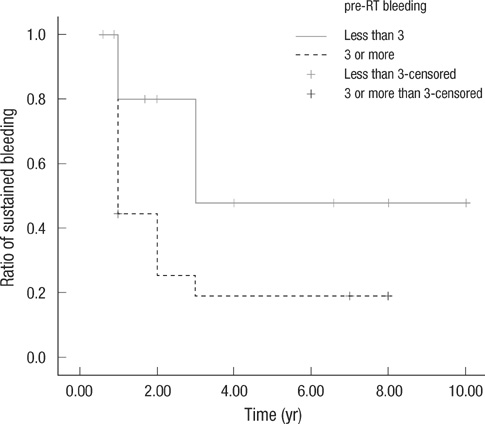
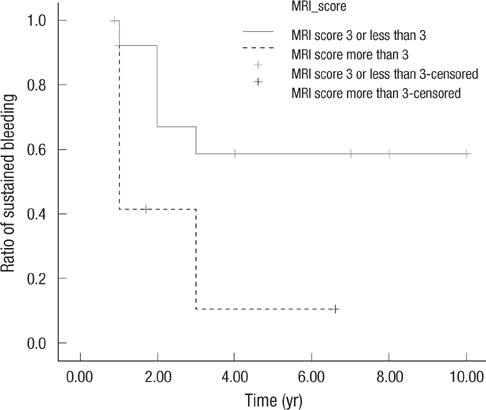
- Bleeding into joint space is critical to develop hemophilic arthropathy. To reduce the frequency of bleeding in the ankle joint of children with hemophilic arthropathy, low dose external beam irradiation was performed for 37 patients. Among them, 35 patients followed-up for longer than 1 yr (median 87 months) were enrolled for analysis. The average number of bleedings per month was 3.6 during one year prior to radiation therapy. After radiation therapy, it was decreased to 2.1 during the first year, after then it was maintained in the range of 1.0 to 1.5 until the tenth year. The bleeding frequency was reduced to 42% at the first year and it was maintained in the range of 58% to 73% from the second to the tenth year. Especially the patients who had 3 or more bleedings per month, and who had MRI score more than 3 showed significant decreases. During the follow-up period, growth disturbances and secondary malignancies were not found. External beam radiotherapy can be considered for the hemophilic patients with surgical or isotope therapies are not amenable.
Keyword
MeSH Terms
Figure
Reference
-
1. Roosendaal G, Lafeber FP. Blood-induced joint damage in hemophilia. Semin Thromb Hemost. 2003. 29:37–42.
Article2. Dunn AL. Management and prevention of recurrent hemarthrosis in patients with hemophilia. Curr Opin Hematol. 2005. 12:390–394.
Article3. Hansen ES, Hjortdal VE, Noer I, Christensen SB, Holm IE, Bunger C. 99mTc-DPD uptake in juvenile hemarthrosis. Scintimetry and autoradiography of the knee in dogs. Orthopedics. 1989. 12:441–447.4. Raffini L, Manno C. Modern management of haemophilic arthropathy. Br J Haematol. 2007. 136:777–787.
Article5. Kang JO, Cho YJ, Yoo MC, Hong SE. Hemophilic pseudotumor of the ulna treated with low dose radiation therapy: a case report. J Korean Med Sci. 2000. 15:601–603.
Article6. Subasi M, Dirier A, Kapukaya A, Uludag A, Karadayi B, Cebesoy O. Successful treatment of hemophilic hand pseudotumors by only radiotherapy. Ann Plast Surg. 2007. 59:338–340.
Article7. Kang JO, Hong SE, Kim SG, Shin DO. The Effect of Radiation Therapy on Hemophilic Arthropathy. J Korean Soc Ther Radiol Oncol. 2005. 23:106–110.8. Arnold WD, Hilgartner MW. Hemophilic arthropathy. Current concepts of pathogenesis and management. J Bone Joint Surg Am. 1977. 59:287–305.
Article9. Funk MB, Schmidt H, Becker S, Escuriola C, Klarmann D, Klingebiel T, Kreuz W. Modified magnetic resonance imaging score compared with orthopaedic and radiological scores for the evaluation of haemophilic arthropathy. Haemophilia. 2002. 8:98–103.
Article10. Jansen NW, Roosendaal G, Lafeber FP. Understanding haemophilic arthropathy: an exploration of current open issues. Br J Haematol. 2008. 143:632–640.
Article11. Roosendaal G, Lafeber F. Prophylactic treatment for prevention of joint disease in hemophilia--cost versus benefit. N Engl J Med. 2007. 357:603–605.12. Kern M, Blanchette V, Stain AM, Einarson TR, Feldman BM. Clinical and cost implications of target joints in Canadian boys with severe hemophilia A. J Pediatr. 2004. 145:628–634.
Article13. Wiedel JD. Arthroscopic synovectomy of the knee in hemophilia: 10-to-15 year followup. Clin Orthop Relat Res. 1996. (328):46–53.14. Luck JV Jr, Silva M, Rodriguez-Merchan EC, Ghalambor N, Zahiri CA, Finn RS. Hemophilic arthropathy. J Am Acad Orthop Surg. 2004. 12:234–245.
Article15. Chang TJ, Mohamed S, Hambleton J. Hemophilic arthropathy: considerations in management. J Am Podiatr Med Assoc. 2001. 91:406–414.
Article16. Mathew P, Talbut DC, Frogameni A, Singer D, Chrissos M, Khuder S, Ohler S, Farley D, Michael C, Robinson MG. Isotopic synovectomy with P-32 in paediatric patients with haemophilia. Haemophilia. 2000. 6:547–555.
Article17. Erken EH. Radiocolloids in the management of hemophilic arthropathy in children and adolescents. Clin Orthop Relat Res. 1991. (264):129–135.
Article18. Gratz S, Gobel D, Behr TM, Herrmann A, Becker W. Correlation between radiation dose, synovial thickness, and efficacy of radiosynoviorthesis. J Rheumatol. 1999. 26:1242–1249.19. Siegel ME, Siegel HJ, Luck JV Jr. Radiosynovectomy's clinical applications and cost effectiveness: a review. Semin Nucl Med. 1997. 27:364–371.
Article20. Silverman CL, Thomas PR, McAlister WH, Walker S, Whiteside LA. Slipped femoral capital epiphyses in irradiated children: dose, volume and age relationships. Int J Radiat Oncol Biol Phys. 1981. 7:1357–1363.
Article21. Hogeboom CJ, Grosser SC, Guthrie KA, Thomas PR, D'Angio GJ, Breslow NE. Stature loss following treatment for Wilms tumor. Med Pediatr Oncol. 2001. 36:295–304.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Radiation Therapy on Hemophilic Arthropathy
- Short-Term Outcomes of Arthroscopic Synovectomy for Hemophilic Ankle Arthropathy
- Radiation Therapy against Pediatric Malignant Central Nervous System Tumors : Embryonal Tumors and Proton Beam Therapy
- Differences in radiotherapy application according to regional disease characteristics of hepatocellular carcinoma
- Hemophilic Arthropathy: Case Report