Ann Lab Med.
2014 Mar;34(2):85-91. 10.3343/alm.2014.34.2.85.
Changes in Plasma Levels of Natural Anticoagulants in Disseminated Intravascular Coagulation: High Prognostic Value of Antithrombin and Protein C in Patients with Underlying Sepsis or Severe Infection
- Affiliations
-
- 1Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Korea. lukekhk@snu.ac.kr
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Laboratory Medicine, Seoul Medical Center, Seoul, Korea.
- KMID: 1791899
- DOI: http://doi.org/10.3343/alm.2014.34.2.85
Abstract
- BACKGROUND
Dysfunctional natural anticoagulant systems enhance intravascular fibrin for mation in disseminated intravascular coagulation (DIC), and plasma levels of natural anti coagulants can be used in the diagnosis and prognosis of DIC. Herein, the diagnostic value of 4 natural anticoagulants was assessed, and the prognostic value of antithrombin and protein C were validated in a large population.
METHODS
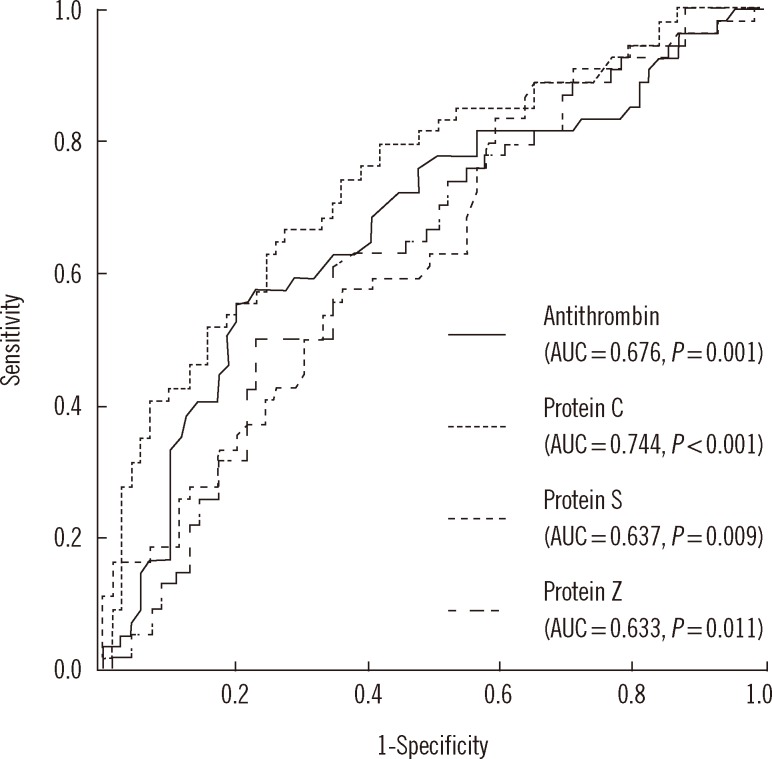
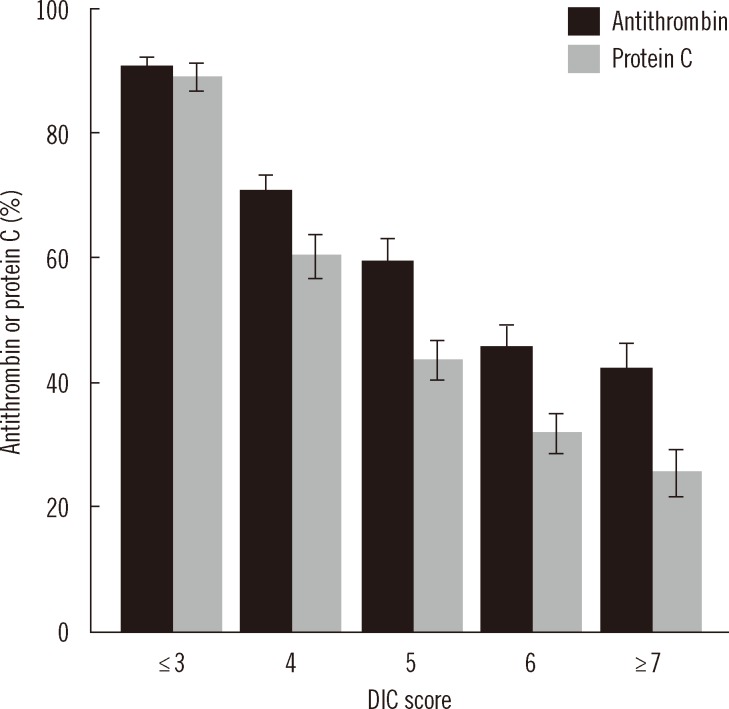
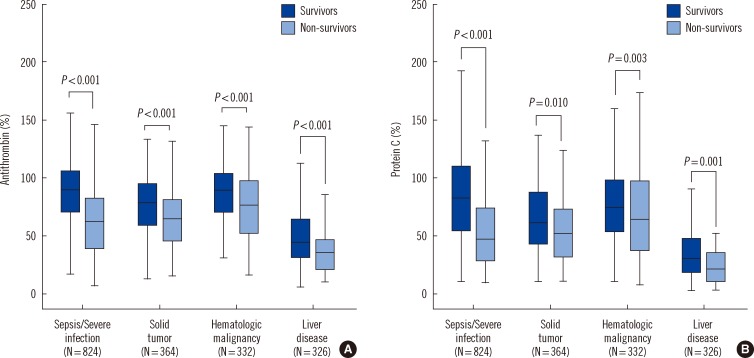
Part 1 study included 126 patients with clinically suspected DIC and estimated plasma levels of 4 candidate anticoagulant proteins: antithrombin, protein C, protein S, and protein Z. Part 2 comprised 1,846 patients, in whom plasma antithrombin and protein C levels were compared with other well-known DIC markers according to the underlying dis eases. The 28-day mortality rate was used to assess prognostic outcome.
RESULTS
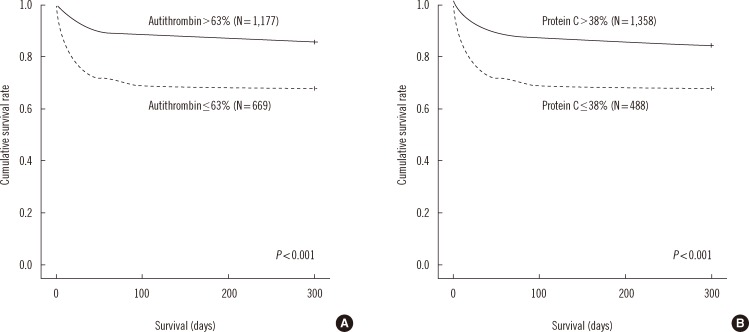
Antithrombin and protein C showed higher areas under the ROC curve than pro tein S and protein Z. In part 2 of the study, antithrombin and protein C levels significantly correlated with DIC score, suggesting that these factors are good indicators of DIC severity. Antithrombin and protein C showed significant prognostic power in Kaplan-Meier analyses. In patients with sepsis/severe infection, antithrombin and protein C showed higher hazard ratios than D-dimer. Platelet count showed the highest hazard ratio in patients with hemato logic malignancy. In patients with liver disease, the hazard ratio for antithrombin levels was significantly high.
CONCLUSIONS
Decreased plasma anticoagulant levels reflect florid consumption of the phys iologic defense system against DIC-induced hypercoagulation. Plasma antithrombin and protein C levels are powerful prognostic markers of DIC, especially in patients with sepsis/severe infection.
Keyword
MeSH Terms
-
Adult
Aged
Anticoagulants/*blood
Antithrombins/*blood
Blood Platelets/cytology
Blood Proteins/analysis
Disseminated Intravascular Coagulation/complications/*diagnosis/mortality
Female
Fibrin Fibrinogen Degradation Products/analysis
Humans
Male
Middle Aged
Platelet Count
Prognosis
Protein C/*analysis
Protein S/analysis
Prothrombin Time
Regression Analysis
Sepsis/complications/*diagnosis
Severity of Illness Index
Anticoagulants
Antithrombins
Blood Proteins
Fibrin Fibrinogen Degradation Products
Protein C
Protein S
Figure
Reference
-
1. Levi M, Toh CH, Thachil J, Watson HG. British Committee for Standards in Haematology. Guidelines for the diagnosis and management of disseminated intravascular coagulation. Br J Haematol. 2009; 145:24–33. PMID: 19222477.
Article2. Sawamura A, Gando S, Hayakawa M, Hoshino H, Kubota N, Sugano M. Effects of antithrombin III in patients with disseminated intravascular coagulation diagnosed by newly developed diagnostic criteria for critical illness. Clin Appl Thromb Hemost. 2009; 15:561–566. PMID: 18840625.
Article3. Fourrier F, Chopin C, Goudemand J, Hendrycx S, Caron C, Rime A, et al. Septic shock, multiple organ failure, and disseminated intravascular coagulation. Compared patterns of antithrombin III, protein C, and protein S deficiencies. Chest. 1992; 101:816–823. PMID: 1531791.4. Macias WL, Nelson DR. Severe protein C deficiency predicts early death in severe sepsis. Crit Care Med. 2004; 32:S223–S228. PMID: 15118522.
Article5. Lauterbach R, Pawlik D, Radziszewska R, Wozniak J, Rytlewski K. Plasma antithrombin III and protein C levels in early recognition of late-onset sepsis in newborns. Eur J Pediatr. 2006; 165:585–589. PMID: 16636814.6. Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Scientific Subcommittee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001; 86:1327–1330. PMID: 11816725.
Article7. Al-Shanqeeti A, van Hylckama Vlieg A, Berntorp E, Rosendaal FR, Broze GJ Jr. Protein Z and protein Z-dependent protease inhibitor. Determinants of levels and risk of venous thrombosis. Thromb Haemost. 2005; 93:411–413. PMID: 15735788.8. Steffano B, Forastiero R, Martinuzzo M, Kordich L. Low plasma protein Z levels in patients with antiphospholipid antibodies. Blood Coagul Fibrinolysis. 2001; 12:411–412. PMID: 11505086.
Article9. Kawasugi K, Wada H, Hatada T, Okamoto K, Uchiyama T, Kushimoto S, et al. Prospective evaluation of hemostatic abnormalities in overt DIC due to various underlying diseases. Thromb Res. 2011; 128:186–190. PMID: 21429565.
Article10. Kaneko T, Wada H. Diagnostic criteria and laboratory tests for disseminated intravascular coagulation. J Clin Exp Hematop. 2011; 51:67–76. PMID: 22104305.
Article11. Levi M, Ten Cate H. Disseminated intravascular coagulation. N Engl J Med. 1999; 341:586–592. PMID: 10451465.
Article12. Maruyama I. Recombinant thrombomodulin and activated protein C in the treatment of disseminated intravascular coagulation. Thromb Haemost. 1999; 82:718–721. PMID: 10605773.
Article13. Chung S, Kim JE, Kim JY, Lee DS, Han KS, Kim HK. Circulating hepatocyte growth factor as an independent prognostic factor of disseminated intravascular coagulation. Thromb Res. 2010; 125:e285–e293. PMID: 20185166.
Article14. Taylor FB, Haddad PA, Hack E, Chang AC, Peer GT, Morrissey JH, et al. Two-stage response to endotoxin infusion into normal human subjects: Correlation of blood phagocyte luminescence with clinical and laboratory markers of the inflammatory, hemostatic response. Crit Care Med. 2001; 29:326–334. PMID: 11269245.
Article15. Kim SY, Kim JE, Kim HK, Kim I, Yoon SS, Park S. Higher prognostic value of soluble fibrin complexes than D-dimer and fibrin degradation product for disseminated intravascular coagulation in patients with liver cirrhosis. Blood Coagul Fibrinolysis. 2013; 24:150–156. PMID: 23314386.
Article16. Corral J, Gonzalez-Conejero R, Hernandez-Espinosa D, Vicente V. Protein Z/Z-dependent protease inhibitor (PZ/ZPI) anticoagulant system and thrombosis. Br J Haematol. 2007; 137:99–108. PMID: 17391489.
Article17. Esmon CT. Protein C anticoagulant system--anti-inflammatory effects. Semin Immunopathol. 2012; 34:127–132. PMID: 21822632.
Article18. Delekta PC, Apel IJ, Gu S, Siu K, Hattori Y, McAllister-Lucas LM, et al. Thrombin-dependent NF-κB activation and monocyte/endothelial adhesion are mediated by the CARMÁ3·Bcl10·MALT signalosome. J Biol Chem. 2010; 285:41432–41442. PMID: 21041303.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Antithrombin III on Disseminated Intravascular Coagulation(DIC) in Premature Infants
- A Clinical Study of Antithrombin lll Therapy for Disseminated Intravascular Coagulation in Neonates
- Use of Antithrombin and Thrombomodulin in the Management of Disseminated Intravascular Coagulation in Patients with Acute Cholangitis
- Studies on Therapeutic Effects and Pathological Features of an Antithrombin Preparation in Septic Disseminated Intravascular Coagulation Patients
- Diagnostic Utility of D-dimer Test in Disseminated Intravascular Coagulation with Sepsis