J Korean Med Sci.
2004 Jun;19(3):453-457. 10.3346/jkms.2004.19.3.453.
Severe Chronic Active EBV Infection in an Adult Patient: Case Report
- Affiliations
-
- 1Department of Pathology, Samsung Medical Center, Sungkyunkwan University, Seoul, Korea. yhko@smc.samsung.co.kr
- 2Department of Hematooncology, Samsung Medical Center, Sungkyunkwan University, Seoul, Korea.
- KMID: 1786827
- DOI: http://doi.org/10.3346/jkms.2004.19.3.453
Abstract
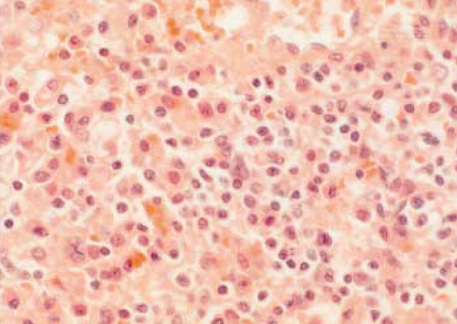
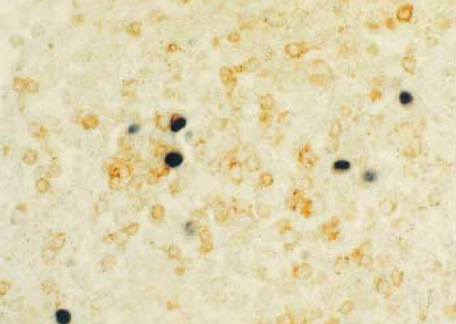
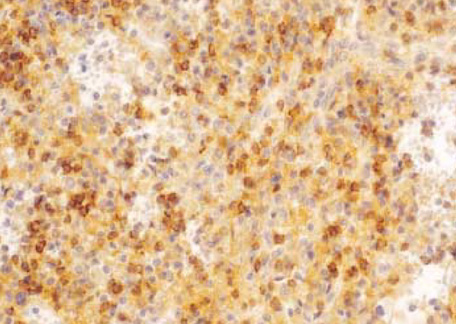
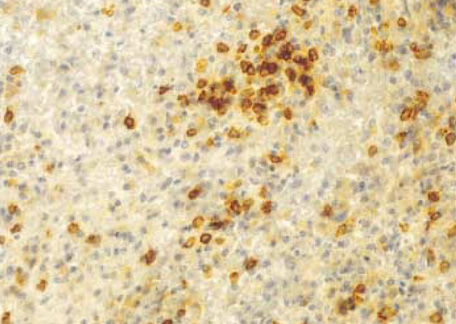
- Severe chronic active Epstein-Barr virus (EBV) infection is a rare and life-threatening illness. Although the criteria for diagnosis include chronic or recurrent infectious mononucleosis-like symptoms lasting more than 6 months and high titers of anti-EBV antibodies, clinical and laboratory findings may be heterogeneous and flexible application of those criteria is necessary in cases showing typical clinical and pathologic findings. We report a case of severe chronic active EBV infection in a 62-yr-old female patient who showed classical clinical findings with infiltration of EBV-infected T lymphocytes in the bone marrow, spleen, and lymph nodes, and died four months after presentation.
MeSH Terms
-
Antigens, CD3/biosynthesis
Antigens, CD4/biosynthesis
Antigens, CD8/biosynthesis
Bone Marrow Cells/virology
Epstein-Barr Virus Infections/*diagnosis/*mortality
Female
Herpesvirus 4, Human/genetics
Human
Immunohistochemistry
Lymph Nodes/virology
Lymphocytes/metabolism
Middle Aged
Organ Weight
Spleen/pathology/virology
Support, Non-U.S. Gov't
T-Lymphocytes/virology
Figure
Reference
-
1. Okano M, Sakiyama Y, Matsumoto S, Mizuno F, Osato T. Unusual lymphoproliferation associated with chronic active Epstein-Barr virus infection. AIDS Res. 1986. 2:Suppl 1. S121–S123.2. Mroczek EC, Weisenburger DD, Grierson HL, Markin R, Purtilo DT. Fatal infectious mononucleosis and virus-associated hemophagocytic syndrome. Arch Pathol Lab Med. 1987. 111:530–535.3. Maia DM, Peace-Brewer AL. Chronic, active Epstein-Barr virus infection. Curr Opin Hematol. 2000. 7:59–63.
Article4. Kasahara Y, Yachie A, Takei K, Kanegane C, Okada K, Ohta K, Seki H, Igarashi N, Maruhashi K, Katayama K, Katoh E, Terao G, Sakiyama Y, Koizumi S. Differential cellular targets of Epstein-Barr virus (EBV) infection between acute EBV-associated hemophagocytic lymphohistiocytosis and chronic active EBV infection. Blood. 2001. 98:1882–1888.
Article5. Kikuta H, Sakiyama Y, Matsumoto S, Oh-Ishi T, Nakano T, Nagashima T, Oka T, Hironaka T, Hirai K. Fatal Epstein-Barr virus-associated hemophagocytic syndrome. Blood. 1993. 82:3259–3264.
Article6. Su IJ, Lin DT, Hsieh HC, Lee SH, Chen J, Chen RL, Lee CY, Chen JY. Fatal primary Epstein-Barr virus infection masquerading as his tiocytic medullary reticulosis in young children in Taiwan. Hematol Pathol. 1990. 4:189–195.7. Purtilo DT, Cassel CK, Yang JP, Harper R. X-linked recessive progressive combined variable immunodeficiency (Duncan's disease). Lancet. 1975. 1:935–940.
Article8. Virelizier JL, Lenoir G, Griscelli C. Persistent Epstein-Barr virus infection in a child with hypergammaglobulinaemia and immunoblastic proliferation associated with a selective defect in immune interferon secretion. Lancet. 1978. 2:231–234.9. Jeong H, Kim BS, Choi OJ, Yoo HW, Lim SD, Hong SJ. A case of chronic active Epstein-Barr virus infection with coronary aneurysm. J Korean Pediatr Soc. 2001. 44:687–693.10. Lee TY, Lee HC, Oh TH, Song BC, Chung YH, Lee YS, Yu ES, Park CJ, Suh DJ. A case of severe chronic active epstein-Barr virus infection with hepatic involvement confirmed by in situ hybridization. Korean J Hepatol. 2001. 7:195–200.11. Straus SE, Tosato G, Armstrong G, Lawley T, Preble OT, Henle W, Davey R, Pearson G, Epstein J, Brus I. Persisting illness and fatigue in adults with evidence of Epstein-Barr virus infection. Ann Intern Med. 1985. 102:7–16.
Article12. Okano M, Matsumoto S, Osato T, Sakiyama Y, Thiele GM, Purtilo DT. Severe chronic active Epstein-Barr virus infection syndrome. Clin Microbiol Rev. 1991. 4:129–135.
Article13. Ishihara S, Okada S, Wakiguchi H, Kurashige T, Morishima T, Kawa-Ha K. Chronic active Epstein-Barr virus infection in children in Japan. Acta Paediatr. 1995. 84:1271–1275.
Article14. Kimura H, Hoshino Y, Kanegane H, Tsuge I, Okamura T, Kawa K, Morishima T. Clinical and virologic characteristics of chronic active Epstein-Barr virus infection. Blood. 2001. 98:280–286.
Article15. Okano M. Overview and problematic standpoints of severe chronic active Epstein-Barr virus infection syndrome. Crit Rev Oncol Hematol. 2002. 44:273–282.
Article16. Ohshima K, Suzumiya J, Sugihara M, Nagafuchi S, Ohga S, Kikuchi M. Clinicopathological study of severe chronic active Epstein-Barr virus infection that developed in association with lymphoproliferative disorder and/or hemophagocytic syndrome. Pathol Int. 1998. 48:934–943.
Article17. Su IJ, Chen RL, Lin DT, Lin KS, Chen CC. Epstein-Barr virus (EBV) infects T lymphocytes in childhood EBV-associated hemophagocytic syndrome in Taiwan. Am J Pathol. 1994. 144:1219–1225.18. Kanegane H, Nomura K, Miyawaki T, Tosato G. Biological aspects of Epstein-Barr virus (EBV)-infected lymphocytes in chronic active EBV infection and associated malignancies. Crit Rev Oncol Hematol. 2002. 44:239–249.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Severe Chronic Active Epstein-Barr Virus Infection with T-cell lymphoproliferative Disorder
- Severe Chronic Active Epstein-Barr Virus Infection Presenting as Fever of Unknown Origin
- A Case of Chronic Active Epstein-Barr Virus Infection with Autoimmnune Hepatitis and a Coronary Aneurysm
- Case of Chronic Active Epstein-Barr Virus Infection Developed Hemophagocytic Lymphohistiocytosis after COVID-19 Infection
- EBV-Associated Lymphoproliferative Disorders