J Korean Med Sci.
2011 Oct;26(10):1386-1390. 10.3346/jkms.2011.26.10.1386.
Mainly Adrenal Gland Involving NK/T-Cell Nasal Type Lymphoma Diagnosed with Delay due to Mimicking Adrenal Hemorrhage
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Research Institute of Clinical Medicine, Chonbuk National University Medical School, Jeonju, Korea. mdjinhy@jbnu.ac.kr
- KMID: 1786000
- DOI: http://doi.org/10.3346/jkms.2011.26.10.1386
Abstract
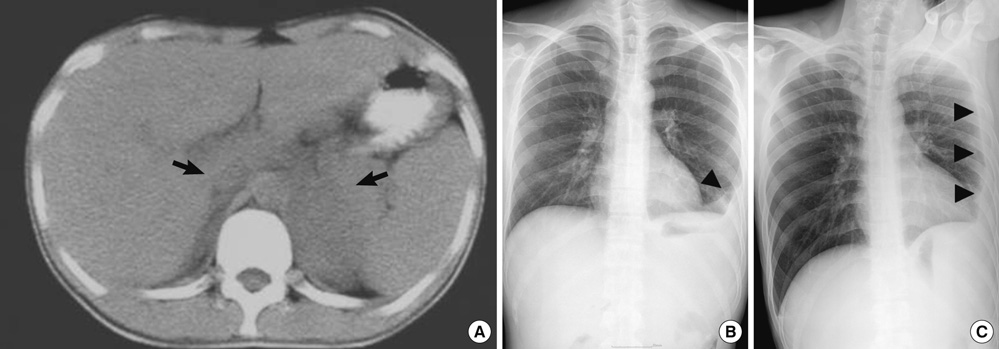
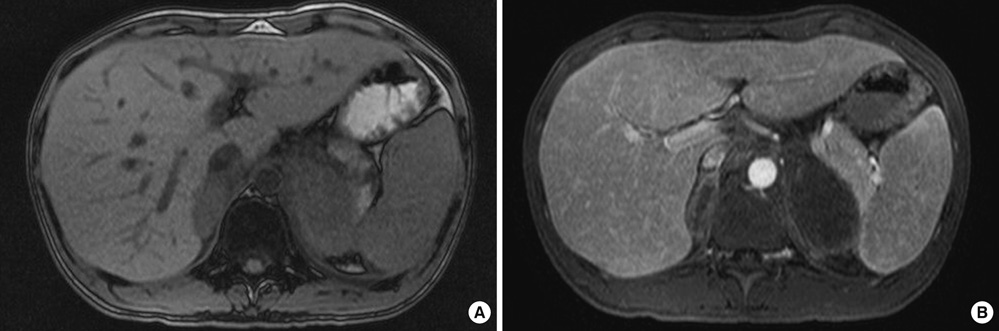
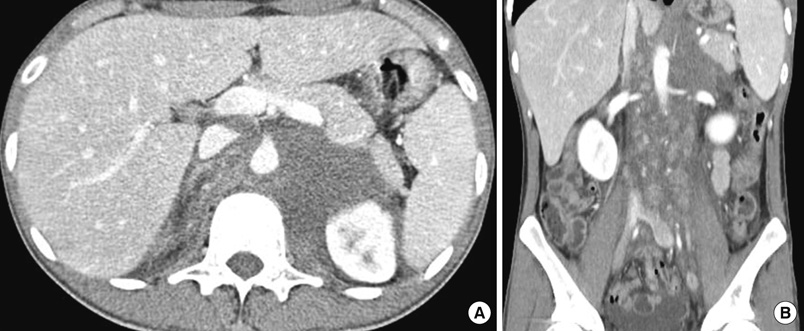
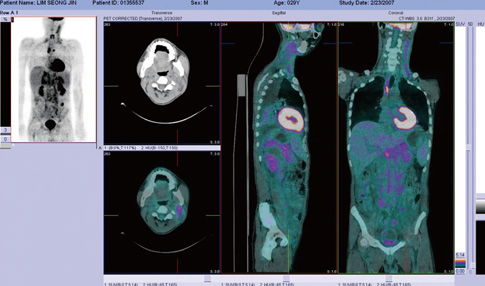
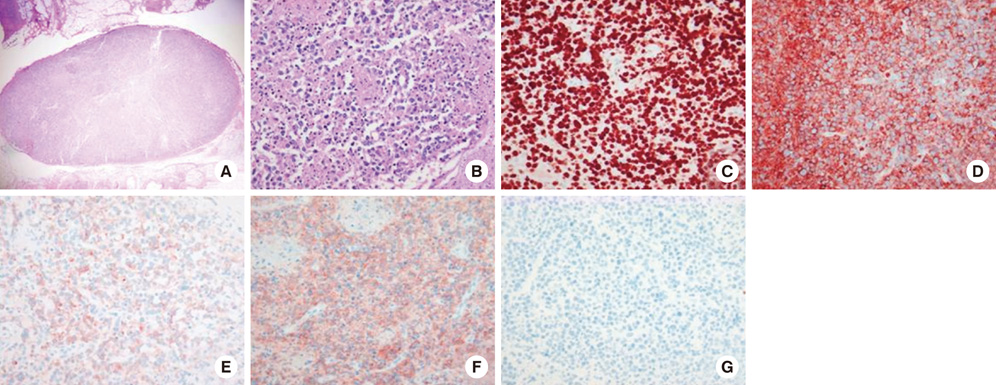
- A 29-yr-old man, presented with abdominal pain and fever, had an initial computed tomography (CT) scan revealing low attenuation of both adrenal glands. The initial concern was for tuberculous adrenalitis or autoimmune adrenalitis combined with adrenal hemorrhage. The patient started empirical anti-tuberculous medication, but there was no improvement. Enlargement of cervical lymph nodes were developed after that and excisional biopsy of cervical lymph nodes was performed. Pathological finding of excised lymph nodes was compatible to NK/T-cell lymphoma. The patient died due to the progression of the disease even after undergoing therapeutic trials including chemotherapy. Lymphoma mainly involving adrenal gland in the early stage of the disease is rare and the vast majority of cases that have been reported were of B-cell origin. From this case it is suggested that extra-nodal NK/T-cell lymphoma should be considered as a cause of bilateral adrenal masses although it is rare.
Keyword
MeSH Terms
Figure
Reference
-
1. AlShemmari SH, Ameen RM, Sajnani KP. Extranodal lymphoma: a comparative study. Hematology. 2008. 13:163–169.2. Rosenberg SA, Diamond HD, Jaslowitz B, Craver LF. Lymphosarcoma: a review of 1269 cases. Medicine (Baltimore). 1961. 40:31–84.3. Mantzios G, Tsirigotis P, Veliou F, Boutsikakis I, Petraki L, Kolovos J, Papageorgiou S, Robos Y. Primary adrenal lymphoma presenting as Addison's disease: case report and review of the literature. Ann Hematol. 2004. 83:460–463.4. Levy NT, Young WF Jr, Habermann TM, Strickler JG, Carney JA, Stanson AW. Adrenal insufficiency as a manifestation of disseminated non-Hodgkin's lymphoma. Mayo Clin Proc. 1997. 72:818–822.5. Grigg AP, Connors JM. Primary adrenal lymphoma. Clin Lymphoma. 2003. 4:154–160.6. van den Heiligenberg SM, van Groeningen CJ. Bilateral adrenal enlargement with an unexpected diagnosis. Eur J Intern Med. 2007. 18:249–250.7. Wang J, Sun NC, Renslo R, Chuang CC, Tabbarah HJ, Barajas L, French SW. Clinically silent primary adrenal lymphoma: a case report and review of the literature. Am J Hematol. 1998. 58:130–136.8. Wang FF, Su CC, Chang YH, Pan CC, Tang KT, Jap TS, Lin HD, Won J. Primary adrenal lymphoma manifestating as adrenal incidentaloma. J Chin Med Assoc. 2003. 66:67–71.9. Arora S, Vargo S, Lupetin AR. Computed tomography appearance of spontaneous adrenal hemorrhage in a pheochromocytoma. Clin Imaging. 2009. 33:314–317.10. Nawar R, Aron D. Adrenal incidentalomas: a continuing management dilemma. Endocr Relat Cancer. 2005. 12:585–598.11. Dunning KK, Wudhikarn K, Safo AO, Holman CJ, McKenna RW, Pambuccian SE. Adrenal extranodal NK/T-cell lymphoma diagnosed by fine-needle aspiration and cerebrospinal fluid cytology and immunophenotyping: a case report. Diagn Cytopathol. 2009. 37:686–695.12. Thompson MA, Habra MA, Routbort MJ, Holsinger FC, Perrier ND, Waguespack SG, Rodriguez MA. Primary adrenal natural killer/T-cell nasal type lymphoma: first case report in adults. Am J Hematol. 2007. 82:299–303.13. Tomoyose T, Nagasaki A, Uchihara JN, Kinjo S, Sugaya K, Onaga T, Ohshima K, Masuda M, Takasu N. Primary adrenal adult T-cell leukemia/lymphoma: a case report and review of the literature. Am J Hematol. 2007. 82:748–752.14. Gopi A, Madhavan SM, Sharma SK, Sahn SA. Diagnosis and treatment of tuberculous pleural effusion in 2006. Chest. 2007. 131:880–889.15. Porcel JM. Tuberculous pleural effusion. Lung. 2009. 187:263–270.16. Ko YH, Ree HJ, Kim WS, Choi WH, Moon WS, Kim SW. Clinicopathologic and genotypic study of extranodal nasal-type natural killer/T-cell lymphoma and natural killer precursor lymphoma among Koreans. Cancer. 2000. 89:2106–2116.17. Lee J, Kim WS, Park YH, Park SH, Park KW, Kang JH, Lee SS, Lee SI, Lee SH, Kim K, Jung CW, Ahn YC, Ko YH, Park K. Nasal-type NK/T cell lymphoma: clinical features and treatment outcome. Br J Cancer. 2005. 92:1226–1230.18. Kohrt H, Advani R. Extranodal natural killer/T-cell lymphoma: current concepts in biology and treatment. Leuk Lymphoma. 2009. 50:1773–1784.19. Mizoguchi Y, Nakamura K, Miyagawa S, Nishimura S, Arihiro K, Kobayashi M. A case of adolescent primary adrenal natural killer cell lymphoma. Int J Hematol. 2005. 81:330–334.20. Kwong YL. Natural killer-cell malignancies: diagnosis and treatment. Leukemia. 2005. 19:2186–2194.