J Korean Acad Periodontol.
2009 Mar;39(1):71-76. 10.5051/jkape.2009.39.1.71.
The effect of non-resorbable barrier membrane on the change of buccal and lingual alveolar bone in immediate implant placement into periapically infected extraction sockets
- Affiliations
-
- 1Department of Periodontics, The Institute of Oral Health Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea. Sb123.kye@samsung.com
- KMID: 1783518
- DOI: http://doi.org/10.5051/jkape.2009.39.1.71
Abstract
-
PURPOSE: Many researches showed loss of alveolar bone in fresh extraction socket and even in case of immediate implant placement. The aim of this study was to evaluate the effect of non-resorbable barrier membrane on the change of buccal and lingual alveolar bone in immediate implant placement into periapically infected extraction sockets.
MATERIALS AND METHODS
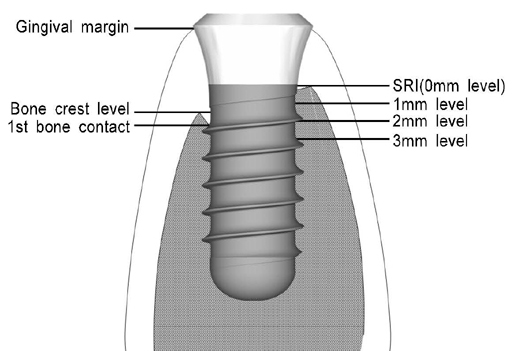
Immediate implants were placed into artificially induced periapical lesion of mandibular premolars after complete debridement using buccal bone defect made by a 6mm trephine bur in 4 mongrel dogs. Before flap repositioning, a non-resorbable barrier membrane was placed on the buccal defect in the experimental group. No membrane was placed in the control group. In 12 weeks after placement, the dogs were sacrificed and undecalcified histologic specimens were prepared. The vertical distance from the smooth-rough surface interface(SRI) to gingiva, 1st bone contact and bone crest were measured in buccal and lingual side. The horizontal thicknesses of gingiva and bone at 0, 1, 2 and 3 mm below SRI were measured.
RESULTS
The buccal bone was resorbed more than lingual bone in both groups and there was statistical significance(p<0.05). The distances from SRI to 1st bone contact were 2.45+/-2.35 mm in experimental group and 4.49+/-3.10 mm in control group. In all vertical level, lingual bone was thicker than buccal bone(p<0.05).
CONCLUSION
Buccal bone was reduced more than lingual bone in immediate implant placement into periapically infected extraction sockets. Placement of non-resorbable barrier membrane reduced the buccal bone resorption. However there was no statistical significance.
Figure
Reference
-
1. Cardaropoli G, Araujo M, Lindhe J. Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J Clin Periodontol. 2003. 30:809–818.2. Carlsson GE, Thilander H, Hedegard B. Histologic changes in the upper alveolar process after extractions with or without insertion of an immediate full denture. Acta Odontol Scand. 1967. 25:21–43.
Article3. Bahat O, Deeb C, Golden T, Komarnyckij O. Preservation of ridges utilizing hydroxyapatite. Int J Periodontics Restorative Dent. 1987. 7:34–41.4. Park J, Kwon Y, Park J, et al. The effect of human demineralized freeze-dried xenograft on vertical bone formation in beagle dogs. J Korean Acad Periodontol. 2008. 38:75–82.
Article5. Seibert JS, Salama H. Alveolar ridge preservation and reconstruction. Periodontol 2000. 1996. 11:69–84.
Article6. Paolantonio M, Dolci M, Scarano A, et al. Immediate implantation in fresh extraction sockets. A controlled clinical and histological study in man. J Periodontol. 2001. 72:1560–1571.
Article7. Araujo MG, Sukekava F, Wennstrom JL, Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol. 2005. 32:645–652.
Article8. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004. 31:820–828.
Article9. Chang SW, Shin SY, Hong JR, et al. Immediate implant placement into infected and noninfected extraction sockets: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 107:197–203.
Article10. Nevins M, Camelo M, De Paoli S, et al. A study of the fate of the buccal wall of extraction sockets of teeth with prominent roots. Int J Periodontics Restorative Dent. 2006. 26:19–29.
Article11. Fickl S, Zuhr O, Wachtel H, Bolz W, Huerzeler MB. Hard tissue alterations after socket preservation: an experimental study in the beagle dog. Clin Oral Implants Res. 2008. 19:1111–1118.
Article12. Antoun H, Sitbon JM, Martinez H, Missika P. A prospective randomized study comparing two techniques of bone augmentation: onlay graft alone or associated with a membrane. Clin Oral Implants Res. 2001. 12:632–639.
Article13. Lorenzoni M, Pertl C, Polansky RA, Jakse N, Wegscheider WA. Evaluation of implants placed with barrier membranes. A restrospective follow-up study up to five years. Clin Oral Implants Res. 2002. 13:274–280.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Benefits of mineralized bone cortical allograft for immediate implant placement in extraction sites: an in vivo study in dogs
- Regeneration of total tissue using alveolar ridge augmentation with soft tissue substitute on periodontally compromised extraction sites: case report
- Immediate implant placement in fresh extraction sockets
- Compromised extraction sockets: a new classification and prevalence involving both soft and hard tissue loss
- EFFECT OF DFDB AND GTAM BARRIERS ON BONE REGENERATION AROUND IMMEDIATE IMPLANTS PLACED IN SURGICALLY DFFECTIVE SOCKET