Infect Chemother.
2012 Feb;44(1):40-43. 10.3947/ic.2012.44.1.40.
A Case of Multiple Pulmonary Nodular Pneumocystis jirovecii Pneumonia in an Acquired Immune Deficiency Syndrome Patient
- Affiliations
-
- 1Department of Internal Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea. songeh@gnah.co.kr
- 2Department of Radiology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 3Department of Pathology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- KMID: 1782398
- DOI: http://doi.org/10.3947/ic.2012.44.1.40
Abstract
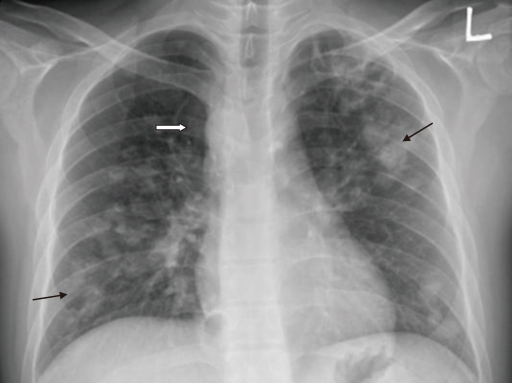
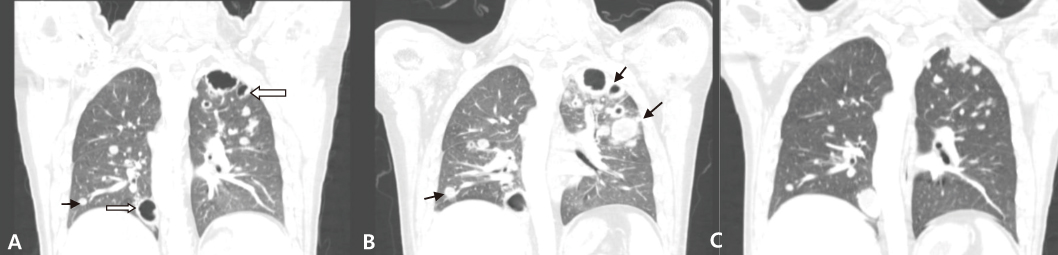
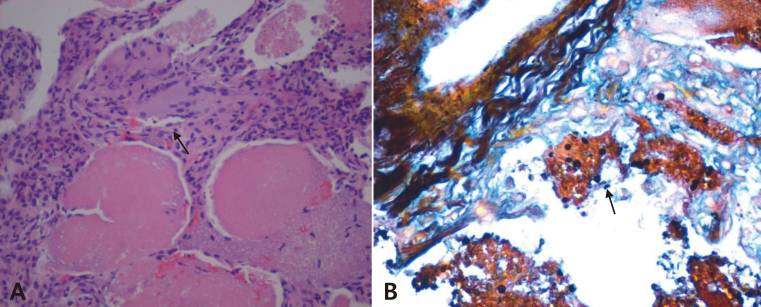
- Pneumocystis jirovecii pneumonia (PCP) is a frequent manifestation of Acquired Immune Deficiency Syndrome (AIDS). The classic chest radiographic finding is perihilar ground glass opacities that may progress to more diffuse lung involvement. Atypical radiographic appearances include a normal chest film, lobar or segmental consolidation, cystic lesions, cavitation, pneumothorax, pleural effusion, and solitary or multiple pulmonary nodules. Although PCP is common in AIDS, presenting with nodular pulmonary densities is rare. We encountered the case of a 33-year-old man with AIDS whose chest radiography showed multiple bilateral nodular patterns suggestive of malignancy. We performed a transcutaneous lung biopsy and diagnosed him with PCP by Gomori methenamine-silver staining. Along with fungal and mycobacterial infections, intrathoracic Kaposi's sarcoma, and lymphoma, PCP should be considered in the differential diagnosis of nodular pulmonary disease in AIDS patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrison's principles of internal medicine. 2008. 17th ed. New York: McGraw-Hill Companies;1137–1204.2. Kim JM, Cho GJ, Hong SK, Chang KH, Chung JS, Choi YH, Song YG, Huh A, Yeom JS, Lee KS, Choi JY. Epidemiology and clinical features of HIV infection/AIDS in Korea. Yonsei Med J. 2003. 44:363–370.
Article3. Klein JS, Warnock M, Webb WR, Gamsu G. Cavitating and noncavitating granulomas in AIDS patients with pneumocystis pneumonitis. AJR Am J Roentgenol. 1989. 152:753–754.
Article4. Winn RA, Stoeckli TC, Wilson ML, Burman W, Schwarz MI, Chan ED. Multiple pulmonary nodules in an HIV-positive man on highly active antiretroviral therapy. Chest. 2002. 122:1840–1843.
Article5. Gallant JE, Ko AH. Cavitary pulmonary lesions in patients infected with human immunodeficiency virus. Clin Infect Dis. 1996. 22:671–682.
Article6. Choe KW, Oh MD, Park SW, Kim HB, Kim US, Kang SW, Choi HJ, Shin DH. Opportunistic infections and malignancies in 173 patients with HIV infection. Korean J Infect Dis. 1998. 30:507–515.7. Shah RM, Salazar AM. CT manifestations of human immunodeficiency virus (HIV)-related pulmonary infections. Semin Ultrasound CT MR. 1998. 19:167–174.
Article8. Kuhlman JE, Kavuru M, Fishman EK, Siegelman SS. Pneumocystis carinii pneumonia: spectrum of parenchymal CT findings. Radiology. 1990. 175:711–714.
Article9. Jasmer RM, Edinburgh KJ, Thompson A, Gotway MB, Creasman JM, Webb WR, Huang L. Clinical and radiographic predictors of the etiology of pulmonary nodules in HIV-infected patients. Chest. 2000. 117:1023–1030.
Article10. Crans CA Jr, Boiselle PM. Imaging features of pneumocystis carinii pneumonia. Crit Rev Diagn Imaging. 1999. 40:251–284.11. Flannery MT, Quiroz E, Grundy LS, Brantley S. Pneumocystis carinii pneumonia with an atypical granulomatous response. South Med J. 1996. 89:409–410.
Article12. Bleiweiss IJ, Jagirdar JS, Klein MJ, Siegel JL, Krellenstein DJ, Gribetz AR, Strauchen JA. Granulomatous pneumocystis carinii pneumonia in three patients with the acquired immune deficiency syndrome. Chest. 1988. 94:580–583.
Article13. Edinburgh KJ, Jasmer RM, Huang L, Reddy GP, Chung MH, Thompson A, Halvorsen RA Jr, Webb RA. Multiple pulmonary nodules in AIDS: usefulness of CT in distinguishing among potential causes. Radiology. 2000. 214:427–432.
Article14. Foley NM, Griffiths MH, Miller RF. Histologically atypical Pneumocystis carinii pneumonia. Thorax. 1993. 48:996–1001.
Article15. Croda J, Croda MG, Neves A, De Sousa dos Santos S. Benefit of antiretroviral therapy on survival of human immunodeficiency virus-infected patients admitted to an intensive care unit. Crit Care Med. 2009. 37:1605–1611.
Article16. Zolopa A, Andersen J, Powderly W, Sanchez A, Sanne I, Suckow C, Hogg E, Komarow L. Early antiretroviral therapy reduces AIDS progression/death in individuals with acute opportunistic infections: a multicenter randomized strategy trial. PLoS ONE. 2009. 4:e5575.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Pneumomediastinum, Pneumopericardium, and Pneumothorax with Respiratory Failure in a Patient with AIDS and Pneumocystis jirovecii Pneumonia
- Unmasking Granulomatous Pneumocystis jirovecii Pneumonia with Nodular Opacity in an HIV-Infected Patient after Initiation of Antiretroviral Therapy
- Pneumocystis jirovecii Pneumonia Accompanied with Fat Embolism: A Case Report
- Acquired immune deficiency syndrome: report of an autopsy case
- Combined Pneumocystis Carinii Pneumonia and Miliary Tuberculosis in a Patient with AIDS