J Korean Med Sci.
2012 Sep;27(9):1109-1113. 10.3346/jkms.2012.27.9.1109.
A Case of Transient Central Diabetes Insipidus after Aorto-Coronary Bypass Operation
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea. sh-park@knu.ac.kr
- 2Clinical Research Center for End Stage Renal Disease, Daegu, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Kyungpook National University Hospital, Daegu, Korea.
- KMID: 1782148
- DOI: http://doi.org/10.3346/jkms.2012.27.9.1109
Abstract
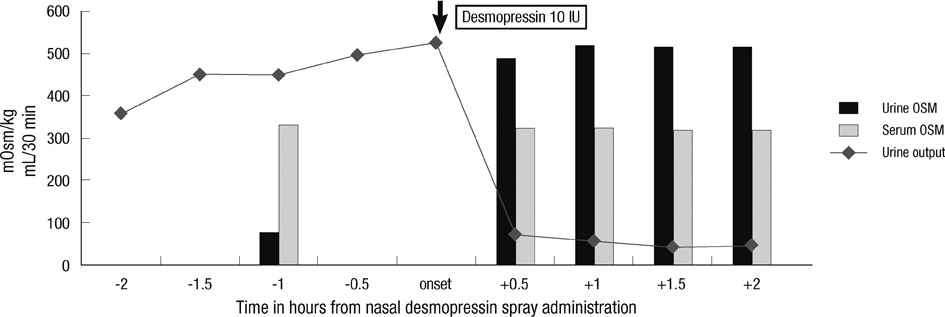
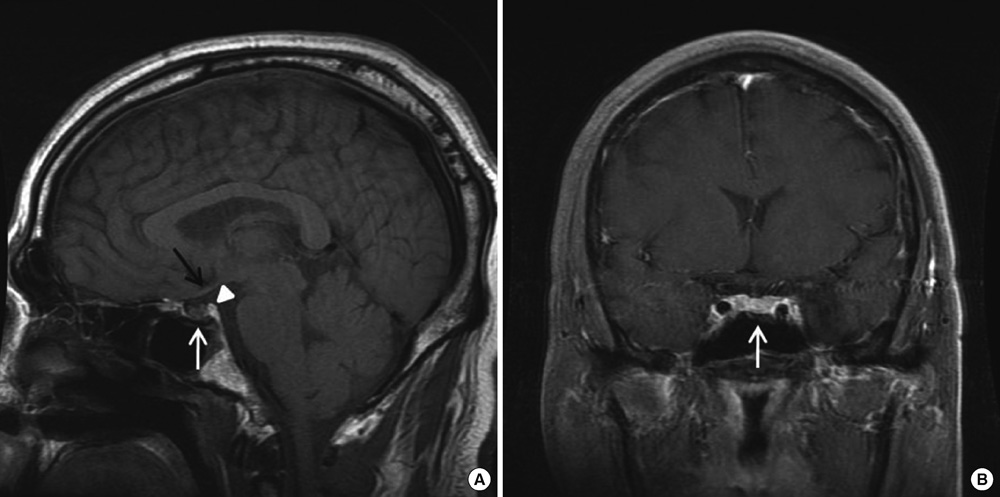
- Diabetes insipidus (DI) is characterized by excessive urination and thirst. This disease results from inadequate output of antidiuretic hormone (ADH) from the pituitary gland or the absence of the normal response to ADH in the kidney. We present a case of transient central DI in a patient who underwent a cardiopulmonary bypass (CPB) for coronary artery bypass grafting (CABG). A 44-yr-old male underwent a CABG operation. An hour after the operation, the patient developed polyuria and was diagnosed with central DI. The patient responded to desmopressin and completely recovered five days after surgery. It is probable that transient cerebral ischemia resulted in the dysfunction of osmotic receptors in the hypothalamus or hypothalamus-pituitary axis during CPB. It is also possible that cardiac standstill altered the left atrial non-osmotic receptor function and suppressed ADH release. Therefore, we suggest that central DI is a possible cause of polyuria after CPB.
MeSH Terms
-
Adult
Antidiuretic Agents/therapeutic use
Coronary Artery Bypass/*adverse effects
Coronary Vessels
Deamino Arginine Vasopressin/therapeutic use
Diabetes Insipidus, Neurogenic/*diagnosis/drug therapy/etiology
Humans
Hypothalamus/radionuclide imaging
Magnetic Resonance Imaging
Male
Pituitary Gland/radionuclide imaging
Polyuria/diagnosis/etiology
Postoperative Complications/*diagnosis/drug therapy/etiology
Antidiuretic Agents
Deamino Arginine Vasopressin
Figure
Reference
-
1. Blotner H. Primary or idiopathic diabetes insipidus: a system disease. Metabolism. 1958. 7:191–200.2. Kuan P, Messenger JC, Ellestad MH. Transient central diabetes insipidus after aortocoronary bypass operations. Am J Cardiol. 1983. 52:1181–1183.3. Ashraf O, Sharif H, Shah M. A case of transient diabetes insipidus following cardiopulmonary bypass. J Pak Med Assoc. 2005. 55:565–566.4. Taylor KM, Wright GS, Reid JM, Bain WH, Caves PK, Walker MS, Grant JK. Comparative studies of pulsatile and nonpulsatile flow during cardiopulmonary bypass. II. The effects on adrenal secretion of cortisol. J Thorac Cardiovasc Surg. 1978. 75:574–578.5. El-Etr AA, Glisson SN. Endocrine changes during anesthesia and cardiopulmonary bypass. Cleve Clin Q. 1981. 48:132–138.6. Philbin DM, Coggins CH, Wilson N, Sokoloski J. Antidiuretic hormone levels during cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1977. 73:145–148.7. Stanley TH, Philbin DM, Coggins CH. Fentanyl-oxygen anesthesia for coronary artery surgery, cardiovascular and antidiuretic hormone response. Can Anaesth Soc J. 1979. 26:168–172.8. Robinson RO, Pagliero KM. Polyruia after cardiac surgery. Br Med J. 1970. 3:265.9. Schrier RW, Berl T, Anderson RJ. Osmotic and nonosmotic control of vasopressin release. Am J Physiol. 1979. 236:F321–F332.10. Schrler RW, Leaf A. Williams RH, editor. Effect of hormones on water, sodium, chloride, and potassium metabolism. Textbook of endocrinology. 1981. 6th ed. Philadelphia: WB Saunders;1032–1037.11. Sheehan HL, Whitehead R. The neurohypophysis in post-partum hypopituitarism. J Pathol Bacteriol. 1963. 85:145–169.12. Sheehan HL, Murdock R. Postpartum necrosis of the anterior pituitary; pathological and clinical aspects. J Obstet Gynaecol Br Commonw. 1938. 45:456–487.13. Breuer AC, Furlan AJ, Hanson MR, Lederman RJ, Loop FD, Cosgrove DM, Greenstreet RL, Estafanous FG. Central nervous system complications of coronary artery bypass graft surgery: prospective analysis of 421 patients. Stroke. 1983. 14:682–687.14. Turnipseed WD, Berkoff HA, Belzer FO. Postoperative stroke in cardiac and peripheral vascular disease. Ann Surg. 1980. 192:365–368.15. Ropper AH, Wechsler LR, Wilson LS. Carotid bruit and the risk of stroke in elective surgery. N Engl J Med. 1982. 307:1388–1390.16. Hart RG, Easton JD. Management of cervical bruits and carotid stenosis in preoperative patients. Stroke. 1983. 14:290–297.17. Reed GL, Singer DE, Pilard EH. Stroke following coronary artery bypass surgery. A case control estimate of the risk of carotid bruits. N Engl J Med. 1988. 319:1246–1250.18. Heikkinen L. Clinically significant neurological disorders following open heart surgery. Thorac Cardiovasc Surg. 1985. 33:201–206.19. Breuer AC, Franco I, Marzewski D, Soto-Velasco J. Left ventricular thrombi seen by ventriculography are a significant risk factor for stroke in open heart surgery. Ann Neurol. 1981. 10:103–104.20. Taylor GJ, Malik SA, Colliver JA, Dove JT, Moses HW, Mikell FL, Batchelder JE, Schneider JA, Wellons HA. Usefulness of atrial fibrillation as a predictor of stroke after isolated coronary artery bypass grafting. Am J Cardiol. 1987. 60:905–907.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Central Diabetes Insipidus Associated with Brachycephaly
- Morphea and Verruca Plana Complicated in Central Diabetes Insipidus
- A Case of Hyperglycemic Hyperosmolar Syndrome in a Patient with Central Diabetes Insipidus and Type 2 Diabetes Mellitus
- Central Diabetes Insipidus Occurring during Therapy for Tsutsugamushi Disease
- A Case of Central Diabetes Insipidus with Growth Hormone Deficiency and Loss of Hyperintense Signal in the Posterior Lobe