Ann Lab Med.
2013 Mar;33(2):97-104. 10.3343/alm.2013.33.2.97.
Therapy-Related Myeloid Neoplasms in 39 Korean Patients: A Single Institution Experience
- Affiliations
-
- 1Department of Laboratory Medicine & Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. heejinkim@skku.edu
- 2Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1781307
- DOI: http://doi.org/10.3343/alm.2013.33.2.97
Abstract
- BACKGROUND
Therapy-related myeloid neoplasms (t-MN) occur as late complications of cytotoxic therapy. This study reviewed clinical and cytogenetic characteristics of patients with t-MN at a single institution in Korea.
METHODS
The study subjects included 39 consecutive patients diagnosed with t-MN. Each subject's clinical history of previous diseases, treatments, and laboratory data was reviewed, including cytogenetics. The primary diagnosis was hematologic malignancy in 14 patients and solid tumor in 25 patients.
RESULTS
Therapy-related acute myeloid leukemia (t-AML, 66.7%) was found to be more common than therapy-related myelodysplastic syndrome (t-MDS). Primary hematologic malignancies that were commonly implicated included mature B-cell neoplasm and acute leukemia. Breast cancer was the most common primary solid tumor. The mean time interval from cytotoxic therapy initiation to t-MN detection was 49 months. Chromosomal aberrations were observed in 35 patients, and loss of chromosome 5, 7, or both accounted for 41% of all cases. Balanced rearrangements occurred in 13 patients; these patients showed shorter latency intervals (mean, 38 months) than patients with loss of chromosome 5 or 7 (mean, 61 months).
CONCLUSIONS
In this study, we determined the clinical and cytogenetic characteristics of Korean patients with t-MN. Although our results were generally consistent with those of previous reports, we found that t-MN resulting from de novo leukemia was common and that t-AML was more common than t-MDS at presentation. Multi-institutional studies involving a larger number of patients and additional parameters are required to investigate the epidemiology, genetic predisposition, and survival rate of t-MN in Korea.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Antineoplastic Agents/*adverse effects/therapeutic use
Asian Continental Ancestry Group
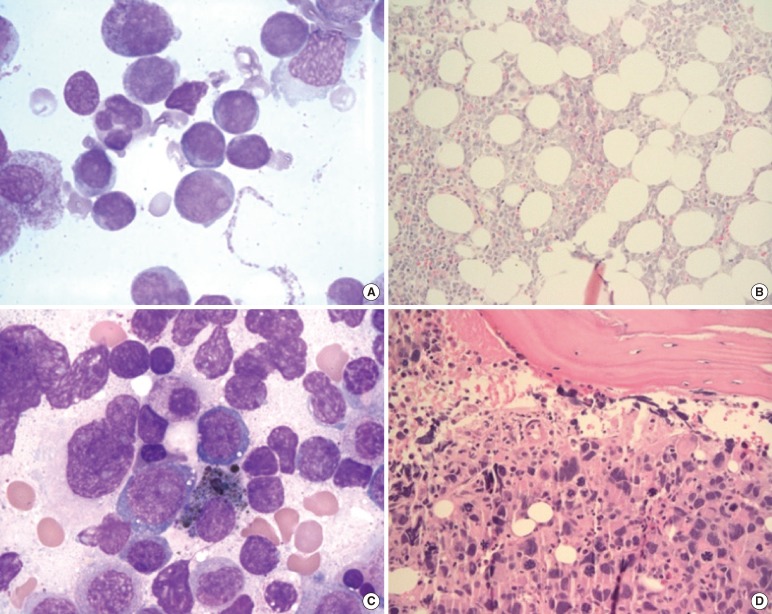
Bone Marrow/pathology
Breast Neoplasms/drug therapy/pathology/radiotherapy
Child
Child, Preschool
Chromosome Aberrations
Chromosomes, Human, Pair 5
Chromosomes, Human, Pair 7
Female
Hematologic Neoplasms/drug therapy/pathology/radiotherapy
Humans
Karyotyping
Leukemia, Myeloid, Acute/*diagnosis/etiology/genetics
Male
Middle Aged
Myelodysplastic Syndromes/*diagnosis/etiology/genetics
Neoplasms, Second Primary/*diagnosis/etiology/genetics
Republic of Korea
Young Adult
Antineoplastic Agents
Figure
Cited by 1 articles
-
Evaluation of prognostic factors in patients with therapy-related acute myeloid leukemia
Sang Hyuk Park, Hyun-Sook Chi, Young-Uk Cho, Seongsoo Jang, Chan-Jeoung Park
Blood Res. 2013;48(3):185-192. doi: 10.5045/br.2013.48.3.185.
Reference
-
1. Swerdlow SH, Campo E, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 2008. 4th ed. Lyon: IARC Press;p. 110.2. Michels SD, McKenna RW, Arthur DC, Brunning RD. Therapy-related acute myeloid leukemia and myelodysplastic syndrome: a clinical and morphologic study of 65 cases. Blood. 1985; 65:1364–1372. PMID: 3857944.
Article3. Le Beau MM, Albain KS, Larson RA, Vardiman JW, Davis EM, Blough RR, et al. Clinical and cytogenetic correlations in 63 patients with therapy-related myelodysplastic syndromes and acute nonlymphocytic leukemia: further evidence for characteristic abnormalities of chromosomes no. 5 and 7. J Clin Oncol. 1986; 4:325–345. PMID: 3950675.
Article4. Smith SM, Le Beau MM, Huo D, Karrison T, Sobecks RM, Anastasi J, et al. Clinical-cytogenetic associations in 306 patients with therapy-related myelodysplasia and myeloid leukemia: the University of Chicago series. Blood. 2003; 102:43–52. PMID: 12623843.
Article5. Rowley JD. International workshop on the relationship of prior therapy to balanced chromosome aberrations in therapy-related myelodysplastic syndromes and acute leukemia: overview report. Genes Chromosomes Cancer. 2002; 33:331–345. PMID: 11921269.
Article6. Rund D, Krichevsky S, Bar-Cohen S, Goldschmidt N, Kedmi M, Malik E, et al. Therapy-related leukemia: clinical characteristics and analysis of new molecular risk factors in 96 adult patients. Leukemia. 2005; 19:1919–1928. PMID: 16167058.
Article7. Pedersen-Bjergaard J. Insights into leukemogenesis from therapy-related leukemia. N Engl J Med. 2005; 352:1591–1594. PMID: 15829541.
Article8. Pedersen-Bjergaard J, Specht L, Larsen SO, Ersbøll J, Struck J, Hansen MM, et al. Risk of therapy-related leukaemia and preleukaemia after Hodgkin's disease. Relation to age, cumulative dose of alkylating agents, and time from chemotherapy. Lancet. 1987; 2:83–88. PMID: 2885581.9. Thirman MJ. Therapy-related myeloid leukemia. Hematol Oncol Clin North Am. 1996; 10:293–320. PMID: 8707757.
Article10. Singh ZN, Huo D, Anastasi J, Smith SM, Karrison T, Le Beau MM, et al. Therapy-related myelodysplastic syndrome: morphologic subclassification may not be clinically relevant. Am J Clin Pathol. 2007; 127:197–205. PMID: 17210514.11. Mauritzson N, Albin M, Rylander L, Billstrom R, Ahlgren T, Mikoczy Z, et al. Pooled analysis of clinical and cytogenetic features in treatment-related and de novo adult acute myeloid leukemia and myelodysplastic syndromes based on a consecutive series of 761 patients analyzed 1976-1993 and on 5098 unselected cases reported in the literature 1974-2001. Leukemia. 2002; 16:2366–2378. PMID: 12454741.
Article12. Pedersen-Bjergaard J, Christiansen DH, Desta F, Andersen MK. Alternative genetic pathways and cooperating genetic abnormalities in the pathogenesis of therapy-related myelodysplasia and acute myeloid leukemia. Leukemia. 2006; 20:1943–1949. PMID: 16990778.
Article13. Estey E, Döhner H. Acute myeloid leukaemia. Lancet. 2006; 368:1894–1907. PMID: 17126723.
Article14. Shaffer LG, Slovak ML, editors. ISCN 2009: An International System of Human Cytogenetic Nomenclature. 2009. Basel: Karger.15. Arana-Yi C, Block AW, Sait SN, Ford LA, Barcos M, Baer MR. Therapy-related myelodysplastic syndrome and acute myeloid leukemia following treatment of acute myeloid leukemia: possible role of cytarabine. Leuk Res. 2008; 32:1043–1048. PMID: 18093651.
Article16. Rund D, Ben-Yehuda D. Therapy-related leukemia and myelodysplasia: evolving concepts of pathogenesis and treatment. Hematology. 2004; 9:179–187. PMID: 15204099.
Article17. Shim H, Chi HS, Jang S, Seo EJ, Park CJ, Lee JH, et al. Therapy-related acute leukemia in breast cancer patients: twelve cases treated with a topoisomerase inhibitor. Korean J Hematol. 2010; 45:177–182. PMID: 21120206.
Article18. Hur M, Lee DS, Shin HY, Ahn HS, Kim BK, Cho HI. Four cases of therapy-related leukemia. J Korean Med Sci. 1999; 14:327–329. PMID: 10402178.
Article19. Lee SY, Kim M, Lim J, Kim Y, Han K, Kim SY, et al. A case of therapy-related acute myeloid leukemia associated with inv(16). Korean J Lab Med. 2007; 27:19–21. PMID: 18094545.
Article20. Seo YI, Park R, Choi TY, Shin JW, Won JH, Park HS, et al. A case of therapy-related acute monocytic leukemia following low-dose of etoposide treatment for hemophagocytic lymphohistiocytosis. Korean J Lab Med. 2007; 27:244–247. PMID: 18094583.
Article21. Park TS, Cheong JW, Song J, Choi JR. Therapy-related myelodysplastic syndrome with der(17)t(12;17)(q13;p13) as a new recurrent cytogenetic abnormality after treatment for chronic lymphocytic leukemia. Leuk Res. 2009; 33:1001–1004. PMID: 19155067.
Article22. Jung CL, Kim HJ, Kim DH, Huh HJ, Song MJ, Kim SH. CKIT mutation in therapy-related acute myeloid leukemia with MLLT3/MLL chimeric transcript from t(9;11)(p22;q23). Ann Clin Lab Sci. 2011; 41:193–196. PMID: 21844580.23. Kim YG, Cho SY, Park TS, Oh SH, Yoon HJ. Therapy-related myelodysplastic syndrome/acute myeloid leukemia with del(7)(q22) in a patient with de novo AML. Ann Clin Lab Sci. 2011; 41:79–83. PMID: 21325260.24. Kwon A, Park JY, Kwon JH, Song HH, Shin KS, Lee YK, et al. A case of therapy-related myeloid neoplasm after successful treatment of acute promyelocytic leukemia. Lab Med Online. 2011; 1:227–231.
Article25. Chandra P, Luthra R, Zuo Z, Yao H, Ravandi F, Reddy N, et al. Acute myeloid leukemia with t(9;11)(p21-22;q23): common properties of dysregulated ras pathway signaling and genomic progression characterize de novo and therapy-related cases. Am J Clin Pathol. 2010; 133:686–693. PMID: 20395514.26. Larson RA. Therapy-related myeloid neoplasms. Haematologica. 2009; 94:454–459. PMID: 19336749.
Article27. Schoch C, Kern W, Schnittger S, Hiddemann W, Haferlach T. Karyotype is an independent prognostic parameter in therapy-related acute myeloid leukemia (t-AML): an analysis of 93 patients with t-AML in comparison to 1091 patients with de novo AML. Leukemia. 2004; 18:120–125. PMID: 14586477.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Therapy-related myeloid neoplasms in children and adolescents
- A case of therapy-related acute myeloid leukemia with inv(16)(p13.1q22) after single low-dose iodine-131 treatment for thyroid cancer
- Clinical characteristics and treatment outcomes of isolated myeloid sarcoma without bone marrow involvement: a single-institution experience
- A Case of Therapy-Related Acute Myeloid Leukemia Following 5-Fluorouracil Chemotherapy
- Intraparenchymal Myeloid Sarcoma and Subsequent Spinal Myeloid Sarcoma for Acute Myeloblastic Leukemia