Yonsei Med J.
2014 Jan;55(1):203-208. 10.3349/ymj.2014.55.1.203.
Inflammatory Cytokine and Osmolarity Changes in the Tears of Dry Eye Patients Treated with Topical 1% Methylprednisolone
- Affiliations
-
- 1Vision Research Institute, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. tikim@yuhs.ac
- KMID: 1779907
- DOI: http://doi.org/10.3349/ymj.2014.55.1.203
Abstract
- PURPOSE
To evaluate changes in clinical outcomes, inflammatory cytokine levels, and tear osmolarity in the tears of patients with moderate to severe dry eye syndrome before and after the application of topical 1% methylprednisolone.
MATERIALS AND METHODS
Thirty-two patients with moderate to severe dry eye unresponsive to previous aqueous enhancement therapy were enrolled. Five patients were lost to follow up, and twenty-seven patients were eligible for analysis. Patients were instructed to apply topical 1% methylprednisolone four times per day, as well as to continue applying their current therapy of preservative-free 0.1% sodium hyaluronate four times per day. Corneal and conjunctival staining scores, tear film breakup time (TFBUT), Schirmer test, and tear osmolarity were assessed at baseline, 4 weeks, and 8 weeks. Tear samples were collected at every visit for cytokine analysis.
RESULTS
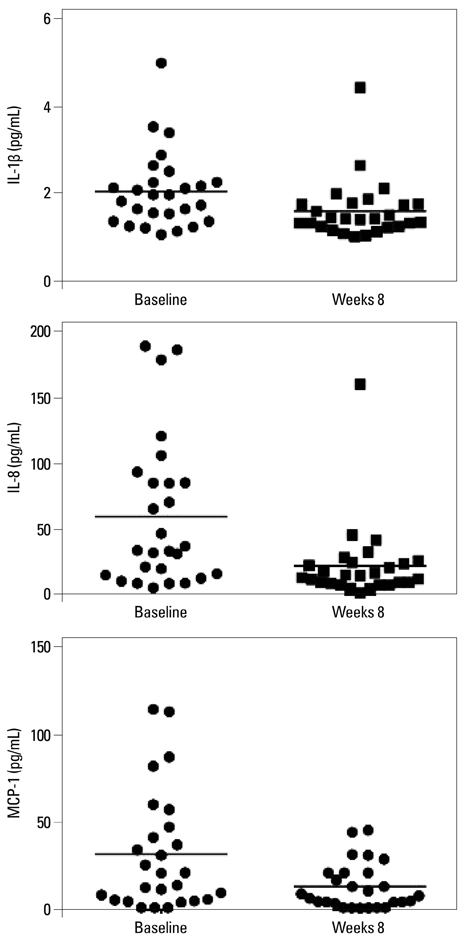
Corneal and conjunctival staining scores and TFBUT showed significant improvement at 4 (p<0.001, <0.001, <0.001 respectively) and 8 (p<0.001, <0.001, <0.001 respectively) weeks. Tear osmolarity decreased significantly at 8 weeks (p=0.008). Interleukin (IL)-1beta, IL-8, and monocyte chemoattractant protein-1 were significantly decreased at 8 weeks compared with those at baseline (p=0.041, 0.001, 0.008 respectively).
CONCLUSION
Short-term treatment with topical 1% methylprednisolone not only improved clinical outcomes, but also decreased tear osmolarity and cytokine levels. By measuring the changes in cytokine levels and tear osmolarity, we could objectively evaluate the anti-inflammatory effects of topical methylprednisolone applied in the treatment of patients with moderate to severe dry eye syndrome.
MeSH Terms
Figure
Reference
-
1. Johnson ME, Murphy PJ. Changes in the tear film and ocular surface from dry eye syndrome. Prog Retin Eye Res. 2004; 23:449–474.
Article2. Lemp MA. Report of the National Eye Institute/Industry workshop on Clinical Trials in Dry Eyes. CLAO J. 1995; 21:221–232.3. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.4. Massingale ML, Li X, Vallabhajosyula M, Chen D, Wei Y, Asbell PA. Analysis of inflammatory cytokines in the tears of dry eye patients. Cornea. 2009; 28:1023–1027.
Article5. Lam H, Bleiden L, de Paiva CS, Farley W, Stern ME, Pflugfelder SC. Tear cytokine profiles in dysfunctional tear syndrome. Am J Ophthalmol. 2009; 147:198–205.
Article6. Yoon KC, Park CS, You IC, Choi HJ, Lee KH, Im SK, et al. Expression of CXCL9, -10, -11, and CXCR3 in the tear film and ocular surface of patients with dry eye syndrome. Invest Ophthalmol Vis Sci. 2010; 51:643–650.
Article7. Suzuki M, Massingale ML, Ye F, Godbold J, Elfassy T, Vallabhajosyula M, et al. Tear osmolarity as a biomarker for dry eye disease severity. Invest Ophthalmol Vis Sci. 2010; 51:4557–4561.
Article8. Sullivan BD, Whitmer D, Nichols KK, Tomlinson A, Foulks GN, Geerling G, et al. An objective approach to dry eye disease severity. Invest Ophthalmol Vis Sci. 2010; 51:6125–6130.
Article9. Stern ME, Gao J, Schwalb TA, Ngo M, Tieu DD, Chan CC, et al. Conjunctival T-cell subpopulations in Sjögren's and non-Sjögren's patients with dry eye. Invest Ophthalmol Vis Sci. 2002; 43:2609–2614.10. Marsh P, Pflugfelder SC. Topical nonpreserved methylprednisolone therapy for keratoconjunctivitis sicca in Sjögren syndrome. Ophthalmology. 1999; 106:811–816.
Article11. Lee HK, Ryu IH, Seo KY, Hong S, Kim HC, Kim EK. Topical 0.1% prednisolone lowers nerve growth factor expression in keratoconjunctivitis sicca patients. Ophthalmology. 2006; 113:198–205.
Article12. Sall K, Stevenson OD, Mundorf TK, Reis BL. CsA Phase 3 Study Group. Two multicenter, randomized studies of the efficacy and safety of cyclosporine ophthalmic emulsion in moderate to severe dry eye disease. Ophthalmology. 2000; 107:631–639.
Article13. De Paiva CS, Corrales RM, Villarreal AL, Farley WJ, Li DQ, Stern ME, et al. Corticosteroid and doxycycline suppress MMP-9 and inflammatory cytokine expression, MAPK activation in the corneal epithelium in experimental dry eye. Exp Eye Res. 2006; 83:526–535.
Article14. Byun YJ, Kim TI, Kwon SM, Seo KY, Kim SW, Kim EK, et al. Efficacy of combined 0.05% cyclosporine and 1% methylprednisolone treatment for chronic dry eye. Cornea. 2012; 31:509–513.
Article15. Tomlinson A, Madden LC, Simmons PA. Effectiveness of dry eye therapy under conditions of environmental stress. Curr Eye Res. 2013; 38:229–236.
Article16. Li DQ, Chen Z, Song XJ, Luo L, Pflugfelder SC. Stimulation of matrix metalloproteinases by hyperosmolarity via a JNK pathway in human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2004; 45:4302–4311.
Article17. Baudouin C. The pathology of dry eye. Surv Ophthalmol. 2001; 45:Suppl 2. S211–S220.
Article18. Lee KY, Rhim JW, Kang JH. Kawasaki disease: laboratory findings and an immunopathogenesis on the premise of a "protein homeostasis system". Yonsei Med J. 2012; 53:262–275.
Article19. Farris RL. Tear osmolarity--a new gold standard? Adv Exp Med Biol. 1994; 350:495–503.20. Liacini A, Sylvester J, Li WQ, Zafarullah M. Inhibition of interleukin-1-stimulated MAP kinases, activating protein-1 (AP-1) and nuclear factor kappa B (NF-kappa B) transcription factors down-regulates matrix metalloproteinase gene expression in articular chondrocytes. Matrix Biol. 2002; 21:251–262.
Article21. Nguyen CQ, Yin H, Lee BH, Chiorini JA, Peck AB. IL17: potential therapeutic target in Sjögren's syndrome using adenovirus-mediated gene transfer. Lab Invest. 2011; 91:54–62.
Article22. Lagu B, Gerchak C, Pan M, Hou C, Singer M, Malaviya R, et al. Potent and selective CC-chemokine receptor-2 (CCR2) antagonists as a potential treatment for asthma. Bioorg Med Chem Lett. 2007; 17:4382–4386.
Article23. Nichols JJ, Sinnott LT. Tear film, contact lens, and patient-related factors associated with contact lens-related dry eye. Invest Ophthalmol Vis Sci. 2006; 47:1319–1328.
Article24. Benelli U, Nardi M, Posarelli C, Albert TG. Tear osmolarity measurement using the TearLab Osmolarity System in the assessment of dry eye treatment effectiveness. Cont Lens Anterior Eye. 2010; 33:61–67.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy and Safety of Topical Unpreserved 0.1% Fluorometholone Ophthalmic Solution on Dry Eye Syndrome
- The Effect of Topical Cyclosporine 0.05% on Tear Osmolarity for Dry Eye Syndrome
- Effect of Sodium Hyaluronate and Cyclosporine A on Tear Film in Dry Eye Syndrome
- Efficacy of Topical Cyclosporine in Mild Dry Eye Patients Having Refractive Surgery
- Comparative Evaluation of Matrix Metalloproteinase-9 Immunoassay and Tear Osmolarity Measurement for Diagnosing Severity of Dry Eye Disease