Yonsei Med J.
2010 Nov;51(6):978-979. 10.3349/ymj.2010.51.6.978.
Claude's Syndrome Associated with Neurocysticercosis
- Affiliations
-
- 1Department of Neurology, JungAng General Hospital, Jeju, Korea.
- 2Department of Radiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Neurology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. kylee@yuhs.ac
- KMID: 1779651
- DOI: http://doi.org/10.3349/ymj.2010.51.6.978
Abstract
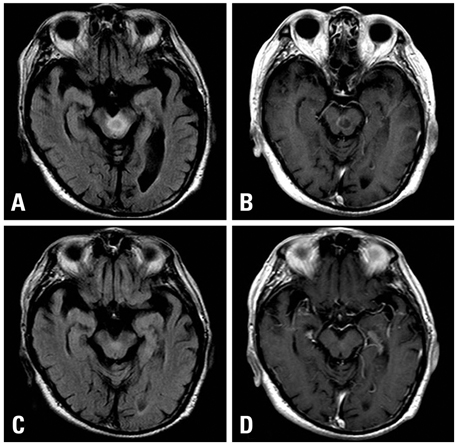
- Claude's syndrome is a distinctive brainstem syndrome characterized by ipsilateral third cranial nerve palsy with contralateral hemiataxia and is due to an intrinsic or extrinsic lesion in the midbrain. We report a case of Claude's syndrome caused by neurocysticercosis infection. A 68 year-old Asian man was admitted to our hospital because of ataxia, left ptosis, and diplopia. Brain magnetic resonance imaging (MRI) showed a cystic lesion in the midbrain, which was surrounded by ring enhancement and peripheral edema. Neurocysticercosis infection was diagnosed by the cerebral spinal fluid study. The patient was treated with albendazole and steroids. A follow-up brain MRI three months later demonstrated the disappearance of a surrounding brain edema and rim enhancement. The most common cause of Claude's syndrome is cerebrovascular disease and malignancy. However, there is no report caused by neurocysticercosis infection. Therefore, if we encounter Claude's syndrome, we should consider neurocysticercosis infection as one of the etiologic factors.
Keyword
MeSH Terms
Figure
Reference
-
1. Del Brutto OH, Rajshekhar V, White AC Jr, Tsang VC, Nash TE, Takayanagui OM, et al. Proposed diagnostic criteria for neurocysticercosis. Neurology. 2001. 57:177–183.
Article2. Katz B. Central American mesencephalopathy. Surv Ophthalmol. 1994. 39:253–259.3. Lath R, Rajshekhar V. Solitary cysticercus granuloma of the brainstem. Report of four cases. J Neurosurg. 1998. 89:1047–1051.4. Sawhney IM, Singh G, Lekhra OP, Mathuriya SN, Parihar PS, Prabhakar S. Uncommon presentations of neurocysticercosis. J Neurol Sci. 1998. 154:94–100.
Article5. Leigh RJ, Zee DS. The neurology of eye movements. 1991. 2nd ed. New York: Oxford University Press.6. Wadley JP, Shakir RA, Rice Edwards JM. Experience with neurocysticercosis in the UK: correct diagnosis and neurosurgical management of the small enhancing brain lesion. Br J Neurosurg. 2000. 14:211–218.
Article7. Mokta JK, Mahajan S, Machhan P, Mokta KK, Patial RK, Prashar BS. Recurrent oculomotor nerve palsy: a rare presentation of neurocysticercosis. Neurol India. 2004. 52:402.8. Kim JS, Jeong SM, Moon SY, Park SH. Third cranial nerve palsy from midbrain neurocysticercosis: repeated exacerbation on tapering corticosteroids. J Neuroophthalmol. 2004. 24:217–220.
Article9. Claude H, Loyez M. Ramollissement du noyau rouge. Rev Neurol. 1924. 41:417–423.10. Kremer C, Baumgartner RW. Aortic embolism in Claude's syndrome. Cerebrovasc Dis. 2002. 13:142–143.
Article11. Seo SW, Heo JH, Lee KY, Shin WC, Chang DI, Kim SM, et al. Localization of Claude's syndrome. Neurology. 2001. 57:2304–2307.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Claude Syndrome in Midbrain Infraction
- Calcified Neurocysticercosis that Invaded the Subarachnoid Space Presenting as Focal Status Epilepticus
- Mesencephalothalamic Lacunar Syndrome Due to Neurocysticercosis
- Extraparenchymal (Racemose) Neurocysticercosis and Its Multitude Manifestations: A Comprehensive Review
- Second Reactivation of Neurocysticercosis: A Case Report