J Clin Neurol.
2015 Jul;11(3):203-211. 10.3988/jcn.2015.11.3.203.
Extraparenchymal (Racemose) Neurocysticercosis and Its Multitude Manifestations: A Comprehensive Review
- Affiliations
-
- 1Department of Neurology, MS Ramaiah Medical College & Hospital, Bangalore, Karnataka, India. rohanmahale83@gmail.com
- KMID: 1894548
- DOI: http://doi.org/10.3988/jcn.2015.11.3.203
Abstract
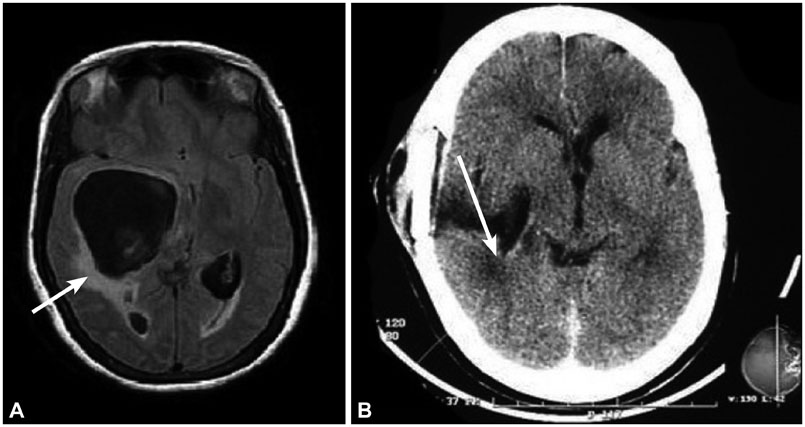
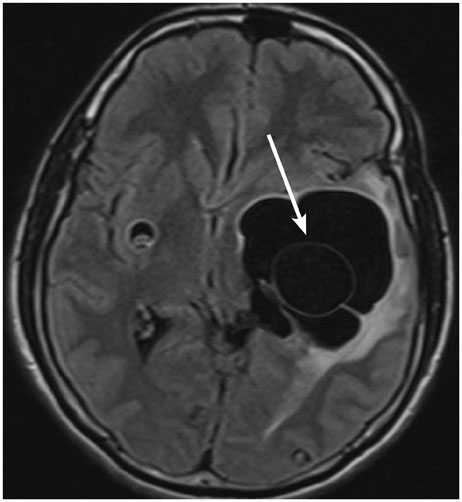
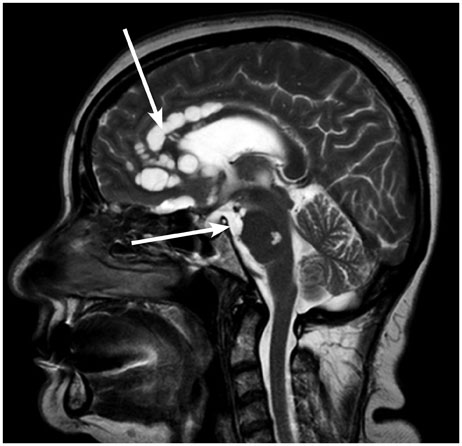
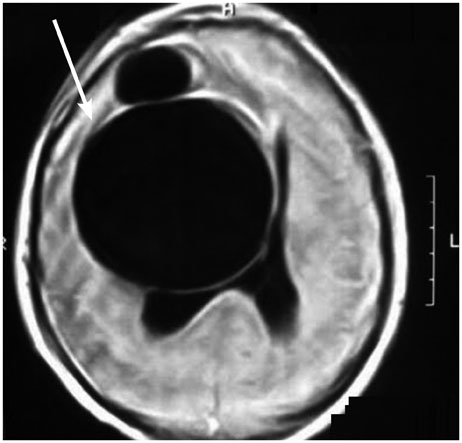
- Neurocysticercosis is an infection of the central nervous system caused by the larval form of the pork tapeworm Taenia solium. In the brain it occurs in two forms: parenchymal and extraparenchymal or racemose cysts. The clinical presentation of racemose cysts is pleomorphic, and is quite different from parenchymal cysticercosis. The clinical diagnosis of racemose cysts is quite challenging, with neuroimaging being the mainstay. However, the advent of newer brain imaging modalities has made a more accurate diagnosis possible. The primary focus of this article is racemose neurocysticercosis and its multitude manifestations, and includes a discussion of the newer diagnostic modalities and treatment options.
Keyword
MeSH Terms
Figure
Reference
-
1. White AC Jr. Neurocysticercosis: updates on epidemiology, pathogenesis, diagnosis, and management. Annu Rev Med. 2000; 51:187–206.
Article2. García HH, Evans CA, Nash TE, Takayanagui OM, White AC Jr, Botero D, et al. Current consensus guidelines for treatment of neurocysticercosis. Clin Microbiol Rev. 2002; 15:747–756.
Article3. Garcia HH, Del Brutto OH. Cysticercosis Working Group in Peru. Neurocysticercosis: updated concepts about an old disease. Lancet Neurol. 2005; 4:653–661.
Article4. Takayanagui OM, Leite JP. [Neurocysticercosis]. Rev Soc Bras Med Trop. 2001; 34:283–290.5. Garcia HH, Gonzales AE, Tsang VC, Gilman RH. The Cysticercosis Working Group in Peru Neurocysticercosis: some of the essentials. Pract Neurol. 2006; 6:288–297.6. Escobar A. The pathology of neurocysticercosis. In : Palacios E, Rodriguez-Carbajal J, Taveras JM, editors. Cysticercosis of the Central Nervous System. Springfield, IL: Charles C. Thomas;1983. p. 27–54.7. Rocca U, Rosell A, Alvarez C. Surgical options in neurocysticercosis therapy. Neurosurg Q. 2005; 15:5–13.
Article8. Kim JH, Suh SI, Kim JH, Kwon TH, Chung HS. Giant neurocysticercosis cyst in the cerebellar hemisphere. Neurol Med Chir (Tokyo). 2006; 46:412–414.9. Zhu L, Shi Y, Pan X, Mo L, Weng X. Successful treatment of isolated cerebellar cysticercosis with albendazole. Chin Med J (Engl). 2003; 116:637–638.10. Martinez HR, Rangel-Guerra R, Elizondo G, Gonzalez J, Todd LE, Ancer J, et al. MR imaging in neurocysticercosis: a study of 56 cases. AJNR Am J Neuroradiol. 1989; 10:1011–1019.11. Khandelwal S, Sakhi P, Sharma GL, Saxena UD. Intraventricular cysticerus. Indian J Radiol Imaging. 2002; 12:329–332.12. Rabiela Cervantes MT, Rivas-Hernandez A, Rodrigues-Ibarra J, Castillo-Medina S, Cancino FM. Anatomopathological aspects of human brain cysticercosis. In : Flisser A, Sillms K, Laclette JP, Larralde C, editors. Cysticercosis: present state of knowledge and perspectives. New York: Academic Press;1982. p. 179–200.13. Couldwell WT, Zee CS, Apuzzo ML. Definition of the role of contemporary surgical management in cisternal and parenchymatous cysticercosis cerebri. Neurosurgery. 1991; 28:231–237.
Article14. Hauptman JS, Hinrichs C, Mele C, Lee HJ. Radiologic manifestations of intraventricular and subarachnoid racemose neurocysticercosis. Emerg Radiol. 2005; 11:153–157.
Article15. Bickerstaff ER, Cloake PC, Hughes B, Smith WT. The racemose form of cerebral cysticercosis. Brain. 1952; 75:1–18.
Article16. Jung RC, Rodriguez MA, Beaver PC, Schenthal JE, Levy RW. Racemose cysticercus in human brain. A case report. Am J Trop Med Hyg. 1981; 30:620–624.17. Sinha S, Sharma BS. Neurocysticercosis: a review of current status and management. J Clin Neurosci. 2009; 16:867–876.
Article18. Apuzzo ML, Dobkin WR, Zee CS, Chan JC, Giannotta SL, Weiss MH. Surgical considerations in treatment of intraventricular cysticercosis. An analysis of 45 cases. J Neurosurg. 1984; 60:400–407.19. Lobato RD, Lamas E, Portillo JM, Roger R, Esparza J, Rivas JJ, et al. Hydrocephalus in cerebral cysticercosis. Pathogenic and therapeutic considerations. J Neurosurg. 1981; 55:786–793.20. Zee CS, Segall HD, Destian S, Ahmadi J, Apuzzo ML. MRI of intraventricular cysticercosis: surgical implications. J Comput Assist Tomogr. 1993; 17:932–939.21. Takayanagui OM, Odashima NS. Clinical aspects of neurocysticercosis. Parasitol Int. 2006; 55:Suppl. S111–S115.
Article22. Colli BO, Martelli N, Assirati JA Jr, Machado HR, de Vergueiro Forjaz S. Surgical treatment of cysticercosis of the central nervous system. Neurosurg Q. 1995; 5:34–35.
Article23. Ghosh D, Dubey TN, Prabhakar S. Brain parenchymal, subarachnoid racemose, and intraventricular cysticercosis in an Indian man. Postgrad Med J. 1999; 75:164–166.
Article24. Pittella JE. Neurocysticercosis. Brain Pathol. 1997; 7:681–693.
Article25. Carpio A. Neurocysticercosis: an update. Lancet Infect Dis. 2002; 2:751–762.
Article26. Sotelo J, Marin C. Hydrocephalus secondary to cysticercotic arachnoiditis. A long-term follow-up review of 92 cases. J Neurosurg. 1987; 66:686–689.27. Joubert J. Cysticercal meningitis--a pernicious form of neurocysticercosis which responds poorly to praziquantel. S Afr Med J. 1990; 77:528–530.28. Keane JR. Cysticercosis: unusual neuro-ophthalmologic signs. J Clin Neuroophthalmol. 1993; 13:194–199.29. Keane JR. Neuro-ophthalmologic signs and symptoms of cysticercosis. Arch Ophthalmol. 1982; 100:1445–1448.
Article30. Stern WE. Neurosurgical considerations of cysticercosis of the central nervous system. J Neurosurg. 1981; 55:382–389.
Article31. Barinagarrementeria F, Del Brutto OH. Lacunar syndrome due to neurocysticercosis. Arch Neurol. 1989; 46:415–417.
Article32. Soto-Hernandez JL, Gomez-Llata Andrade S, Rojas-Echeverri LA, Texeira F, Romero V. Subarachnoid hemorrhage secondary to a ruptured inflammatory aneurysm: a possible manifestation of neurocysticercosis: case report. Neurosurgery. 1996; 38:197–199. discussion 199-200
Article33. Rodriguez-Carbajal J, Del Brutto OH, Penagos P, Huebe J, Escobar A. Occlusion of the middle cerebral artery due to cysticercotic angiitis. Stroke. 1989; 20:1095–1099.
Article34. Sawhney IM, Singh G, Lekhra OP, Mathuriya SN, Parihar PS, Prabhakar S. Uncommon presentations of neurocysticercosis. J Neurol Sci. 1998; 154:94–100.
Article35. Barinagarrementeria F, Cantú C. Frequency of cerebral arteritis in subarachnoid cysticercosis: an angiographic study. Stroke. 1998; 29:123–125.
Article36. Hawk MW, Shahlaie K, Kim KD, Theis JH. Neurocysticercosis: a review. Surg Neurol. 2005; 63:123–132. discussion 132
Article37. Rocha MS, Brucki SM, Ferraz AC, Piccolo AC. [Cerebrovascular disease and neurocysticercosis]. Arq Neuropsiquiatr. 2001; 59:778–783.38. Jankowski R, Zimmerman RD, Leeds NE. Cysticercosis presenting as a mass lesion at foramen of Monro. J Comput Assist Tomogr. 1979; 3:694–696.
Article39. King JS, Hosobuchi Y. Cysticercus cyst of the lateral ventricle. Surg Neurol. 1977; 7:125–129.40. Cuetter AC, Andrews RJ. Intraventricular neurocysticercosis: 18 consecutive patients and review of the literature. Neurosurg Focus. 2002; 12:e5.
Article41. Diehl Rodriquez R, Crestani DN, Dworzecki Soares JO, Franceshini PR, Petersen Alves R, Zimerman R, et al. Bruns' syndrome and racemose neurocysticercosis: a case report. Rev Soc Bras Med Trop. 2012; 45:269–271.
Article42. Torres-Corzo J, Rodriguez-della Vecchia R, Rangel-Castilla L. Bruns syndrome caused by intraventricular neurocysticercosis treated using flexible endoscopy. J Neurosurg. 2006; 104:746–748.
Article43. Krasnianski M, Müller T, Stock K, Zierz S. Bruns syndrome caused by intraventricular tumor. Eur J Med Res. 2008; 13:179–181.44. Sharma S, Modi M, Lal V, Prabhakar S, Bhardwaj A, Sehgal R. Reversible dementia as a presenting manifestation of racemose neurocysticercosis. Ann Indian Acad Neurol. 2013; 16:88–90.
Article45. Ciampi de Andrade D, Rodrigues CL, Abraham R, Castro LH, Livramento JA, Machado LR, et al. Cognitive impairment and dementia in neurocysticercosis: a cross-sectional controlled study. Neurology. 2010; 74:1288–1295.
Article46. Ramirez-Bermudez J, Higuera J, Sosa AL, Lopez-Meza E, Lopez-Gomez M, Corona T. Is dementia reversible in patients with neurocysticercosis? J Neurol Neurosurg Psychiatry. 2005; 76:1164–1166.
Article47. Forlenza OV, Filho AH, Nobrega JP, dos Ramos Machado L, de Barros NG, de Camargo CH, et al. Psychiatric manifestations of neurocysticercosis: a study of 38 patients from a neurology clinic in Brazil. J Neurol Neurosurg Psychiatry. 1997; 62:612–616.
Article48. Kumar S, Thakur S, Jhobta A, Sood RG. Giant racemose neurocysticercosis with mass effect: unusual presentation. Ann Indian Acad Neurol. 2013; 16:398–399.
Article49. Kim SW, Kim MK, Oh SM, Park SH. Racemose cysticercosis in the cerebellar hemisphere. J Korean Neurosurg Soc. 2010; 48:59–61.
Article50. Ahmad FU, Sharma BS. Treatment of intramedullary spinal cysticercosis: report of 2 cases and review of literature. Surg Neurol. 2007; 67:74–77. discussion 77
Article51. Bandres JC, White AC Jr, Samo T, Murphy EC, Harris RL. Extraparenchymal neurocysticercosis: report of five cases and review of management. Clin Infect Dis. 1992; 15:799–811.
Article52. De Souza Queiroz L, Filho AP, Callegaro D, De Faria LL. Intramedullary cysticercosis. Case report, literature review and comments on pathogenesis. J Neurol Sci. 1975; 26:61–70.53. Sharma BS, Banerjee AK, Kak VK. Intramedullary spinal cysticercosis. Case report and review of literature. Clin Neurol Neurosurg. 1987; 89:111–116.54. Corral I, Quereda C, Moreno A, López-Vélez R, Martínez-San-Millán J, Guerrero A, et al. Intramedullary cysticercosis cured with drug treatment. A case report. Spine (Phila Pa 1976). 1996; 21:2284–2287.55. Canas NM, Calado SL, Vale J. [Treatment of racemose neurocysticercosis of the spine]. Rev Neurol. 2005; 40:544–547.56. Wadia RS, Makhale CN, Kelkar AV, Grant KB. Focal epilepsy in India with special reference to lesions showing ring or disc-like enhancement on contrast computed tomography. J Neurol Neurosurg Psychiatry. 1987; 50:1298–1301.
Article57. Nash TE, Neva FA. Recent advances in the diagnosis and treatment of cerebral cysticercosis. N Engl J Med. 1984; 311:1492–1496.
Article58. Salazar A, Sotelo J, Martinez H, Escobedo F. Differential diagnosis between ventriculitis and fourth ventricle cyst in neurocysticercosis. J Neurosurg. 1983; 59:660–663.
Article59. Wallin MT, Kurtzke JF. Neurocysticercosis in the United States: review of an important emerging infection. Neurology. 2004; 63:1559–1564.
Article60. Castillo M. Imaging of neurocysticercosis. Semin Roentgenol. 2004; 39:465–473.
Article61. do Amaral LL, Ferreira RM, da Rocha AJ, Ferreira NP. Neurocysticercosis: evaluation with advanced magnetic resonance techniques and atypical forms. Top Magn Reson Imaging. 2005; 16:127–144.62. Govindappa SS, Narayanan JP, Krishnamoorthy VM, Shastry CH, Balasubramaniam A, Krishna SS. Improved detection of intraventricular cysticercal cysts with the use of three-dimensional constructive interference in steady state MR sequences. AJNR Am J Neuroradiol. 2000; 21:679–684.63. Robbani I, Razdan S, Pandita KK. Diagnosis of intraventricular cysticercosis by magnetic resonance imaging: improved detection with three-dimensional spoiled gradient recalled echo sequences. Australas Radiol. 2004; 48:237–239.
Article64. Rangel-Guerra RA, Herrera J, Elizondo G, Gonzalez-Morantes J. Neurocysticercosis. Arch Neurol. 1988; 45:492.
Article65. Schantz PM, Tsang VC, Maddison SE. Serodiagnosis of neurocysticercosis. Rev Infect Dis. 1988; 10:1231–1233.
Article66. Tsang VC, Brand JA, Boyer AE. An enzyme-linked immunoelectrotransfer blot assay and glycoprotein antigens for diagnosing human cysticercosis (Taenia solium). J Infect Dis. 1989; 159:50–59.
Article67. Wilson M, Bryan RT, Fried JA, Ware DA, Schantz PM, Pilcher JB, et al. Clinical evaluation of the cysticercosis enzyme-linked immunoelectrotransfer blot in patients with neurocysticercosis. J Infect Dis. 1991; 164:1007–1009.
Article68. Rosas N, Sotelo J, Nieto D. ELISA in the diagnosis of neurocysticercosis. Arch Neurol. 1986; 43:353–356.
Article69. Nguekam , Zoli AP, Ongolo-Zogo P, Dorny P, Brandt J, Geerts S. Follow-up of neurocysticercosis patients after treatment using an antigen detection ELISA. Parasite. 2003; 10:65–68.
Article70. Garcia HH, Parkhouse RM, Gilman RH, Montenegro T, Bernal T, Martinez SM, et al. Serum antigen detection in the diagnosis, treatment, and follow-up of neurocysticercosis patients. Trans R Soc Trop Med Hyg. 2000; 94:673–676.
Article71. Correa D, Sandoval MA, Harrison LJ, Parkhouse RM, Plancarte A, Meza-Lucas A, et al. Human neurocysticercosis: comparison of enzyme immunoassay capture techniques based on monoclonal and polyclonal antibodies for the detection of parasite products in cerebrospinal fluid. Trans R Soc Trop Med Hyg. 1989; 83:814–816.
Article72. Harrison LJ, Joshua GW, Wright SH, Parkhouse RM. Specific detection of circulating surface/secreted glycoproteins of viable cysticerci in Taenia saginata cysticercosis. Parasite Immunol. 1989; 11:351–370.
Article73. Garcia HH, Harrison LJ, Parkhouse RM, Montenegro T, Martinez SM, Tsang VC, et al. A specific antigen-detection ELISA for the diagnosis of human neurocysticercosis. The Cysticercosis Working Group in Peru. Trans R Soc Trop Med Hyg. 1998; 92:411–414.
Article74. Fleury A, Hernández M, Avila M, Cárdenas G, Bobes RJ, Huerta M, et al. Detection of HP10 antigen in serum for diagnosis and follow-up of subarachnoidal and intraventricular human neurocysticercosis. J Neurol Neurosurg Psychiatry. 2007; 78:970–974.
Article75. Singh G. Neurocysticercosos in South-Central America and the Indian subcontinent. A comparative evaluation. Arq Neuropsiquiatr. 1997; 55:349–356.
Article76. Carpio A, Santillán F, León P, Flores C, Hauser WA. Is the course of neurocysticercosis modified by treatment with antihelminthic agents? Arch Intern Med. 1995; 155:1982–1988.
Article77. Kramer LD. Medical treatment of cysticercosis--ineffective. Arch Neurol. 1995; 52:101–102.
Article78. Salinas R, Prasad K. Drugs for treating neurocysticercosis (tapeworm infection of the brain). Cochrane Database Syst Rev. 2000; CD000215.
Article79. Sotelo J, del Brutto OH, Penagos P, Escobedo F, Torres B, Rodriguez-Carbajal J, et al. Comparison of therapeutic regimen of anticysticercal drugs for parenchymal brain cysticercosis. J Neurol. 1990; 237:69–72.
Article80. Sotelo J, Del Brutto OH. Review of neurocysticercosis. Neurosurg Focus. 2002; 12:e1.
Article81. Proaño JV, Madrazo I, García L, García-Torres E, Correa D. Albendazole and praziquantel treatment in neurocysticercosis of the fourth ventricle. J Neurosurg. 1997; 87:29–33.
Article82. Göngora-Rivera F, Soto-Hernández JL, González Esquivel D, Cook HJ, Márquez-Caraveo C, Hernández Dávila R, et al. Albendazole trial at 15 or 30 mg/kg/day for subarachnoid and intraventricular cysticercosis. Neurology. 2006; 66:436–438.
Article83. Proaño JV, Madrazo I, Avelar F, López-Félix B, Díaz G, Grijalva I. Medical treatment for neurocysticercosis characterized by giant subarachnoid cysts. N Engl J Med. 2001; 345:879–885.
Article84. Del Brutto OH. Albendazole therapy for subarachnoid cysticerci: clinical and neuroimaging analysis of 17 patients. J Neurol Neurosurg Psychiatry. 1997; 62:659–661.
Article85. Mitre E, Talaat KR, Sperling MR, Nash TE. Methotrexate as a corticosteroid-sparing agent in complicated neurocysticercosis. Clin Infect Dis. 2007; 44:549–553.
Article86. Colli BO, Martelli N, Assirati JA Jr, Machado HR, de Vergueiro Forjaz S. Results of surgical treatment of neurocysticercosis in 69 cases. J Neurosurg. 1986; 65:309–315.
Article87. Kelley R, Duong DH, Locke GE. Characteristics of ventricular shunt malfunctions among patients with neurocysticercosis. Neurosurgery. 2002; 50:757–761. discussion 761-762
Article88. Sharma BS, Gupta SK, Khosla VK. Neurocysticercosis: surgical considerations. Neurol India. 1998; 46:177–182.89. Husain M, Jha D, Vatsal DK, Thaman D, Gupta A, Husain N, et al. Neuro-endoscopic surgery--experience and outcome analysis of 102 consecutive procedures in a busy neurosurgical centre of India. Acta Neurochir (Wien). 2003; 145:369–375. discussion 375-37690. Husain M, Rastogi M, Jha DK, Husain N, Gupta RK. Endoscopic transaqueductal removal of fourth ventricular neurocysticercosis with an angiographic catheter. Neurosurgery. 2007; 60:4 Suppl 2. 249–253. discussion 254
Article91. Anandh B, Mohanty A, Sampath S, Praharaj SS, Kolluri S. Endoscopic approach to intraventricular cysticercal lesions. Minim Invasive Neurosurg. 2001; 44:194–196.
Article92. Cudlip SA, Wilkins PR, Marsh HT. Endoscopic removal of a third ventricular cysticercal cyst. Br J Neurosurg. 1998; 12:452–454.
Article93. Madrazo I, García-Rentería JA, Sandoval M, López Vega FJ. Intraventricular cysticercosis. Neurosurgery. 1983; 12:148–152.
Article94. Neal JH. An endoscopic approach to cysticercosis cysts of the posterior third ventricle. Neurosurgery. 1995; 36:1040–1043.
Article95. Bergsneider M. Endoscopic removal of cysticercal cysts within the fourth ventricle. Technical note. J Neurosurg. 1999; 91:340–345.96. Bergsneider M, Holly LT, Lee JH, King WA, Frazee JG. Endoscopic management of cysticercal cysts within the lateral and third ventricles. J Neurosurg. 2000; 92:14–23.
Article97. Psarros TG, Krumerman J, Coimbra C. Endoscopic management of supratentorial ventricular neurocysticercosis: case series and review of the literature. Minim Invasive Neurosurg. 2003; 46:331–334.
Article98. Husain M, Jha DK, Rastogi M, Husain N, Gupta RK. Neuro-endoscopic management of intraventricular neurocysticercosis (NCC). Acta Neurochir (Wien). 2007; 149:341–346.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neuroimaging Findings in Racemose Neurocysticercosis: Case Description and Literature Review
- Cerebral Parenchymal Racemose Cysticercosis
- A Case of Neurocysticercosis Presenting with Myelopathy and Hydrocephalus
- Neurocysticercosis-Surgical and Medical Management with Praziquantel
- Neurocysticercosis: Clinical Characteristics and Changes from 26 Years of Experience in an University Hospital in Korea