Korean J Pain.
2012 Apr;25(2):81-88. 10.3344/kjp.2012.25.2.81.
Evaluation of an Experimentally Designed Stereotactic Guidance System for Determining Needle Entry Point during Uniplanar Fluoroscopy-guided Intervention
- Affiliations
-
- 1Department of Biomedical Engineering, School of Medicine, Pusan National University, Yangsan, Korea.
- 2Department of Anesthesia and Pain Medicine, School of Medicine, Pusan National University, Yangsan, Korea. pain@pusan.ac.kr
- KMID: 1778990
- DOI: http://doi.org/10.3344/kjp.2012.25.2.81
Abstract
- BACKGROUND
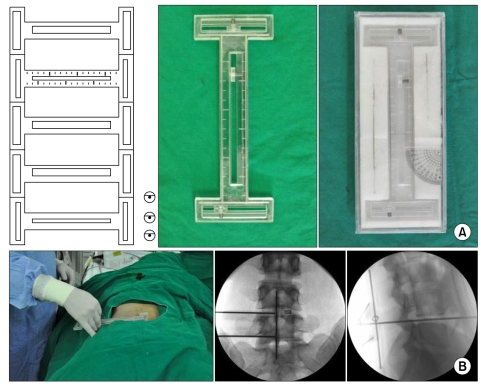
In discography performed during percutaneous endoscopic lumbar discectomy (PELD) via the posterolateral approach, it is difficult to create a fluoroscopic tunnel view because a long needle is required for discography and the guide-wire used for consecutive PELD interrupts rotation of fluoroscope. A stereotactic system was designed to facilitate the determination of the needle entry point, and the feasibility of this system was evaluated during interventional spine procedures.
METHODS
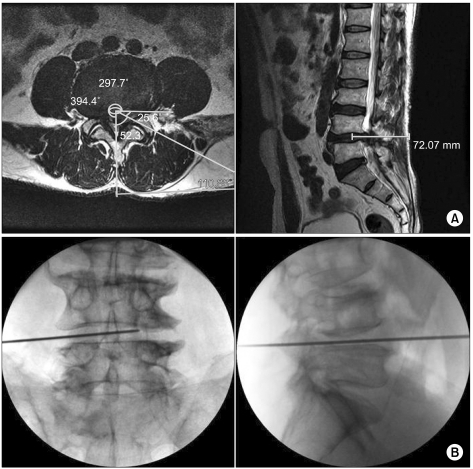
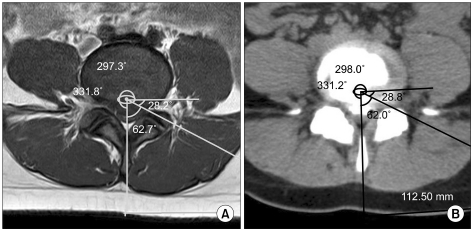
A newly designed stereotactic guidance system underwent a field test application for PELD. Sixty patients who underwent single-level PELD at L4-L5 were randomly divided into conventional or stereotactic groups. PELD was performed via the posterolateral approach using the entry point on the skin determined by premeasured distance from the midline and angles according to preoperative magnetic resonance imaging (MRI) findings. Needle entry accuracy provided by the two groups was determined by comparing the distance and angle measured by postoperative computed tomography with those measured by preoperative MRI. The duration and radiation exposure for determining the entry point were measured in the groups.
RESULTS
The new stereotactic guidance system and the conventional method provided similarly accurate entry points for discography and consecutive PELD. However, the new stereotactic guidance system lowered the duration and radiation exposure for determining the entry point.
CONCLUSIONS
The new stereotactic guidance system under fluoroscopy provided a reliable needle entry point for discography and consecutive PELD. Furthermore, it reduced the duration and radiation exposure associated with determining needle entry.
MeSH Terms
Figure
Cited by 1 articles
-
Percutaneous osteoplasty for painful bony lesions: a technical survey
Won-Sung Kim, Kyung-Hoon Kim
Korean J Pain. 2021;34(4):375-393. doi: 10.3344/kjp.2021.34.4.375.
Reference
-
1. Park MS, Lee KM, Lee B, Min E, Kim Y, Jeon S, et al. Comparison of operator radiation exposure between C-arm and O-arm fluoroscopy for orthopaedic surgery. Radiat Prot Dosimetry. 2012; 148:431–438. PMID: 21525041.
Article2. von Jako RA, Cselik Z. Percutaneous laser discectomy guided with stereotactic computer-assisted surgical navigation. Lasers Surg Med. 2009; 41:42–51. PMID: 19143018.
Article3. Best NM, Sasso RC, Garrido BJ. Computer-assisted spinal navigation using a percutaneous dynamic reference frame for posterior fusions of the lumbar spine. Am J Orthop (Belle Mead NJ). 2009; 38:387–391. PMID: 19809603.4. Kim KH, Kim IS. Kim DH, Kim KH, Kim YC, editors. Current understanding of spinal pain and the nomenclature of lumbar disc pathology. Minimally invasive percutaneous spinal techniques. 2010. Philadelphia: Elsevier/Saunders;p. 44.
Article5. Ropper AE, Chi JH. Maximal radiation exposure during minimally invasive spine surgery? Neurosurgery. 2011; 68:N23–N24. PMID: 21792103.6. Kim KH. Use of lidocaine patch for percutaneous endoscopic lumbar discectomy. Korean J Pain. 2011; 24:74–80. PMID: 21716614.
Article7. Harned ME, Owen RD, Steyn PG, Hatton KW. Novel use of intraoperative dexmedetomidine infusion for sedation during spinal cord stimulator lead placement via surgical laminectomy. Pain Physician. 2010; 13:19–22. PMID: 20119459.8. Yeung AT. The evolution of percutaneous spinal endoscopy and discectomy: state of the art. Mt Sinai J Med. 2000; 67:327–332. PMID: 11021785.9. Tian NF, Huang QS, Zhou P, Zhou Y, Wu RK, Lou Y, et al. Pedicle screw insertion accuracy with different assisted methods: a systematic review and meta-analysis of comparative studies. Eur Spine J. 2011; 20:846–859. PMID: 20862593.
Article10. Tjardes T, Shafizadeh S, Rixen D, Paffrath T, Bouillon B, Steinhausen ES, et al. Image-guided spine surgery: state of the art and future directions. Eur Spine J. 2010; 19:25–45. PMID: 19763640.
Article11. Tonn JC, Schichor C, Schnell O, Zausinger S, Uhl E, Morhard D, et al. Intraoperative computed tomography. Acta Neurochir Suppl. 2011; 109:163–167. PMID: 20960337.
Article12. Schlenzka D, Laine T, Lund T. Computer-assisted spine surgery. Eur Spine J. 2000; 9(Suppl 1):S57–S64. PMID: 10766059.
Article13. Jolesz FA. Future perspectives for intraoperative MRI. Neurosurg Clin N Am. 2005; 16:201–213. PMID: 15561539.
Article14. Specht LM, Koval KJ. Robotics and computer-assisted orthopaedic surgery. Bull Hosp Jt Dis. 2001-2002; 60:168–172. PMID: 12102405.15. Barzilay Y, Liebergall M, Fridlander A, Knoller N. Miniature robotic guidance for spine surgery--introduction of a novel system and analysis of challenges encountered during the clinical development phase at two spine centres. Int J Med Robot. 2006; 2:146–153. PMID: 17520625.
Article16. Ishikawa Y, Kanemura T, Yoshida G, Matsumoto A, Ito Z, Tauchi R, et al. Intraoperative, full-rotation, three-dimensional image (O-arm)-based navigation system for cervical pedicle screw insertion. J Neurosurg Spine. 2011; 15:472–478. PMID: 21761967.
Article17. Abul-Kasim K, Söderberg M, Selariu E, Gunnarsson M, Kherad M, Ohlin A. Optimization of radiation exposure and image quality of the cone-beam O-arm intraoperative imaging system in spinal surgery. J Spinal Disord Tech. 2012; 25:52–58. PMID: 21423057.
Article18. Oertel MF, Hobart J, Stein M, Schreiber V, Scharbrodt W. Clinical and methodological precision of spinal navigation assisted by 3D intraoperative O-arm radiographic imaging. J Neurosurg Spine. 2011; 14:532–536. PMID: 21275555.
Article19. Kim KH, Kim TK. Kim DH, Kim KH, Kim YC, editors. Unipedicular approach for percutaneous vertebroptasty. 2010. Philadelphia: Elsevier/Saunders;p. 270–276.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy and Safety in Pedicle Screw Placement in the Thoracic and Lumbar Spines : Comparison Study between Conventional C-Arm Fluoroscopy and Navigation Coupled with O-Arm(R) Guided Methods
- The Validation of Ultrasound-Guided Lumbar Facet Nerve Blocks as Confirmed by Fluoroscopy
- Fluoroscope guided epidural needle insertioin in midthoracic region: clinical evaluation of Nagaro's method
- Ultrasound-Guided Intervention in Lumbar Spine
- An Alternative Approach to Needle Placement in Cervicothoracic Epidural Injections