Yonsei Med J.
2006 Dec;47(6):833-839. 10.3349/ymj.2006.47.6.833.
Surgical Experiences of Functioning Neuroendocrine Neoplasm of the Pancreas
- Affiliations
-
- 1Department of Surgery, Yonsei University, College of Medicine, Seoul, Korea. wjlee@yumc.younsei.ac.kr
- KMID: 1777173
- DOI: http://doi.org/10.3349/ymj.2006.47.6.833
Abstract
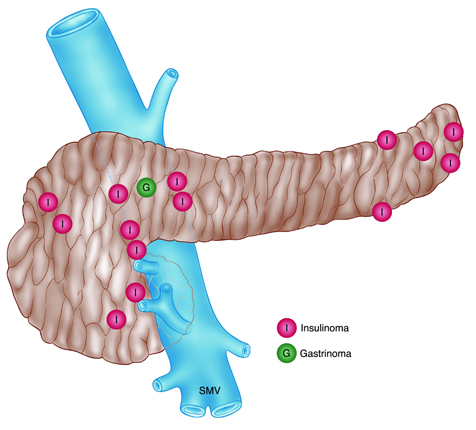
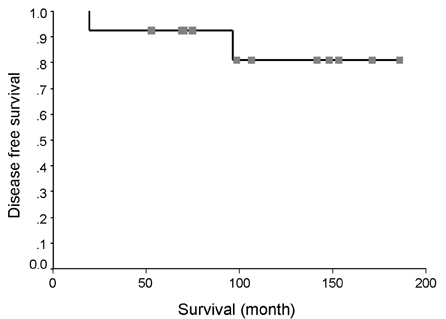
- We present our surgical experiences with functioning neuroendocrine neoplasms of the pancreas to define its natural history, and to suggest its proper management. From June 1990 to June 2005, patients with diagnosis of functioning neuroendocrine (islet cell) neoplasms of the pancreas were retrospectively reviewed. Fourteen patients (5 men and 9 women) with a median age of 49 years (range, 12 - 68 years) were identified. Twelve patients (86%) had insulinoma, two (14%) had gastrinoma. One (7%) with pancreatic insulinoma was multiple endocrine neoplasia type 1. Intraoperative ultrasound scan (sensitivity, 83%) was the most powerful modality for tumor localization. Fifteen neoplasms with median tumor size 1 cm (range 0-3 cm) were resected. Four insulinomas (26.7%) were located in the head of the pancreas and 5 (36%), in the tail. Another 5 (36%) insulinomas and 1 (7%) gastrinoma were located around the neck area near the SMV or PV. Eleven patients (79%) underwent enucleation, and 2 patients (14%), distal pancreatectomy with splenectomy. 100% of patients with functioning neuroendocrine neoplasms of the pancreas have survived. The overall disease free 10-year survival was found to be about 81%. Exact localization of tumor by intraoperative ultrasound and surgical removal are promising for good prognosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Delcore R, Friesen SR. Gastrointestinal neuroendocrine tumors. J Am Coll Surg. 1994. 178:187–211.2. Azimuddin K, Chamberlain RS. The surgical management of pancreatic neuroendocrine tumors. Surg Clin North Am. 2001. 81:511–525.3. Matthews BD, Smith TI, Kercher KW, Holder WD Jr, Heniford BT. Surgical experience with functioning pancreatic neuroendocrine tumors. Am Surg. 2002. 68:660–666.4. Phan GQ, Yeo CJ, Hruban RH, Lillemoe KD, Pitt HA, Cameron JL. Surgical experience with pancreatic and peripancreatic neuroendocrine tumor: review of 125 patients. J Gastrointest Surg. 1998. 2:472–482.5. Akerstrom G, Hellman P, Hessman O, Osmak L. Surgical treatment of endocrine pancreatic tumors. Neuroendocrinology. 2004. 80:Suppl 1. 62–66.6. Anderson MA, Carpenter S, Thompson NW, Nostrant TT, Elta GH, Scheiman JM. Endoscopic ultrasound is highly accurate and directs management in patients with neuroendocrine tumors of the pancreas. Am J Gastroenterol. 2000. 95:2271–2277.7. Thompson NW, Czako PF, Fritts LL, Bude R, Bansal R, Nostrant TT, et al. Role of endoscopic ultrasonography in the localization of insulinomas and gastrinomas. Surgery. 1994. 116:1131–1138.8. Grant CS, van Heerden J, Charboneau JW, James EM, Reading CC. Insulinoma: the value of intraoperative ultrasonography. Arch Surg. 1998. 123:843–848.9. Howard TJ, Stabile BE, Zinner MJ, Chang S, Bhagavan BS, Passaro E Jr. Anatomic distribution of pancreatic endocrine tumors. Am J Surg. 1990. 159:258–264.10. Gagner M, Inabnet WB, Biertho L, Salky B. Laparoscopic pancreatectomy: a series of 22 patients. Ann Chir. 2004. 129:2–10.11. Melvin WS, Needleman BJ, Krause KR, Eliision EC. Robotic resection of pancreatic neuroendocrine tumor. J Laparoendosc Adv Surg Tech A. 2003. 13:33–36.12. Yu F, Venzon DJ, Serrano J, Goebel SU, Doppman JL, Gibri F, et al. Prospective study of the clinical course, prognostic factors, causes of death, and survival in patients with long-standing Zollinger-Ellison syndrome. J Clin Oncol. 1999. 17:615–630.13. Heitz PU, Kasper M, Polak JM, Kloppel G. Pancreatic endocrine tumours. Hum Pathol. 1982. 13:263–271.14. Lairmore TC, Moley JF. Townsend CM, Beaychamp RD, Evers BM, Matthox KL, editors. The multiple endocrine neoplasia syndromes. Sabiston textbook of surgery: The Biological Basis of Modern Surgical Practice. 2004. 17th ed. Philadelphia: Elsevier Saunders;1071–1087.15. Kim YW, Park YK, Park JH, Lee SH, Lee J, Ko SW, et al. Iselt cell hyperplasia of the pancreas presenting as hperinsulinemic hypoglycemia in an adult. Yonsei Med J. 2000. 41:426–429.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Experiences of Neuroendocrine Neoplasms of the Pancreas : Comparative Study of Functioning vs. Non-functioning Neoplasms
- Laparoscopic Enucleation of a Nonfunctioning Neuroendocrine Tumor of the Pancreas
- Single Institutional Experiences of Insulinoma
- Pancreas Neuroendocrine Tumor and Its Mimics: Review of Cross-Sectional Imaging Findings for Differential Diagnosis
- A Case of Pancreatic Neuroendocrine Tumor Mimicked Intraductal Papillary Mucinous Neoplasm