Yonsei Med J.
2011 May;52(3):543-546. 10.3349/ymj.2011.52.3.543.
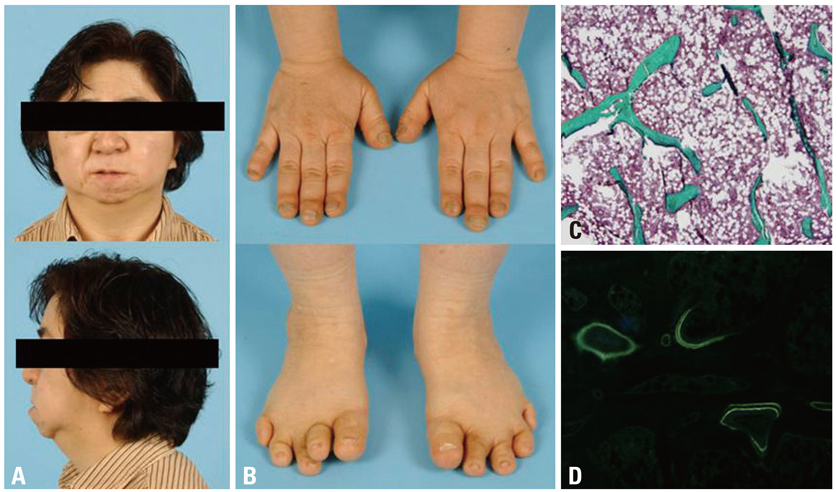
Effect of Zoledronic Acid on Acro-Osteolysis and Osteoporosis in a Patient with Hajdu-Cheney Syndrome
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. yumie@yuhs.ac
- 2Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Radiology, Ajou University College of Medicine, Suwon, Korea.
- KMID: 1777031
- DOI: http://doi.org/10.3349/ymj.2011.52.3.543
Abstract
- Hajdu-Cheney syndrome is a rare, autosomal dominant skeletal dysplasia marked by acro-osteolysis of the distal phalanges and severe osteoporosis. Although there are more than 60 reports published to date, proper treatment and subsequent outcome have been scarce. Herein, we report a progress of anti-resorptive therapy with zoledronic acid, in a woman with Hajdu-Cheney syndrome. Results suggest that anti-resorptive therapy may be important in delaying the progress of osteoporosis and preventing fractures, but not necessarily acro-osteolysis itself.
Keyword
MeSH Terms
Figure
Reference
-
1. Hajdu N, Kauntze R. Cranio-skeletal dysplasia. Br J Radiol. 1948. 21:42–48.
Article2. Cheney WD. Acro-osteolysis. Am J Roentgenol Radium Ther Nucl Med. 1965. 94:595–607.3. Diren HB, Kovanlikaya I, Süller A, Dicle O. The Hajdu-Cheney syndrome: a case report and review of the literature. Pediatr Radiol. 1990. 20:568–569.
Article4. Nunziata V, di Giovanni G, Ballanti P, Bonucci E. High turnover osteoporosis in acro-osteolysis (Hajdu-Cheney syndrome). J Endocrinol Invest. 1990. 13:251–255.
Article5. Leidig-Bruckner G, Pfeilschifter J, Penning N, Limberg B, Priemel M, Delling G, et al. Severe osteoporosis in familial Hajdu-Cheney syndrome: progression of acro-osteolysis and osteoporosis during long-term follow-up. J Bone Miner Res. 1999. 14:2036–2041.
Article6. Udell J, Schumacher HR Jr, Kaplan F, Fallon MD. Idiopathic familial acroosteolysis: histomorphometric study of bone and literature review of the Hajdu-Cheney syndrome. Arthritis Rheum. 1986. 29:1032–1038.
Article7. Won YY, Chung YS, Park YK, Yoo VY. Correlations between microcomputed tomography and bone histomorphometry in Korean young females. Yonsei Med J. 2003. 44:811–815.
Article8. Han EJ, Mun JI, An SY, Jung YJ, Kim OH, Chung YS. A Case Report of Hajdu-Cheney Syndrome. Endocrinol Metab. 2010. 25:152–156.
Article9. Kawamura J, Matsubayashi K, Ogawa M. Hadju-Cheney syndrome. Report of a non-familial case. Neuroradiology. 1981. 21:295–301.
Article10. Brennan AM, Pauli RM. Hajdu--Cheney syndrome: evolution of phenotype and clinical problems. Am J Med Genet. 2001. 100:292–310.
Article11. Marik I, Kuklik M, Zemkowa D, Kozlowski K. Hajdu-Cheney syndrome: report of a family and a short literature review. Australas Radiol. 2006. 50:534–538.
Article12. Brown DM, Bradford DS, Gorlin RJ, Desnick RJ, Langer LO, Jowsey J, et al. The acro-osteolysis syndrome: Morphologic and biochemical studies. J Pediatr. 1976. 88:573–580.
Article13. Iwaya T, Taniguchi K, Watanabe J, Iinuma K, Hamazaki Y, Yoshikawa S. Hajdu-Cheney syndrome. Arch Orthop Trauma Surg. 1979. 95:293–302.
Article14. Lifchus-Ascher RJ, Tucci JR. Hajdu-Cheney syndrome in a 19-year-old man. Endocr Pract. 2006. 12:690–694.
Article15. Drake WM, Hiorns MP, Kendler DL. Hadju-Cheney syndrome: response to therapy with bisphosphonates in two patients. J Bone Miner Res. 2003. 18:131–133.
Article16. McKiernan FE. Integrated anti-remodeling and anabolic therapy for the osteoporosis of Hajdu-Cheney syndrome. Osteoporos Int. 2007. 18:245–249.
Article17. McKiernan FE. Integrated anti-remodeling and anabolic therapy for the osteoporosis of Hajdu-Cheney syndrome: 2-year follow-up. Osteoporos Int. 2008. 19:379–380.
Article18. Al-Mayouf SM, Madi SM, Bin-Abbas BS. Cyclic intravenous pamidronate treatment in children with nodulosis, arthropathy and osteolysis syndrome. Ann Rheum Dis. 2006. 65:1672–1673.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of Hajdu-Cheney Syndrome
- An Unusual Presentation of Diabetic Ketoacidosis in Familial Hajdu-Cheney Syndrome: A Case Report
- Band acro-osteolysis in a Black woman: a case report and review of the literature
- A case of acro-osteolysis caused by peripheral neuropathy after minor burn injury
- Intravenous Zoledronic Acid in Elderly Patients with Benign Paroxysmal Positional Vertigo and Osteoporosis