Arch Hand Microsurg.
2022 Mar;27(1):62-67. 10.12790/ahm.21.0140.
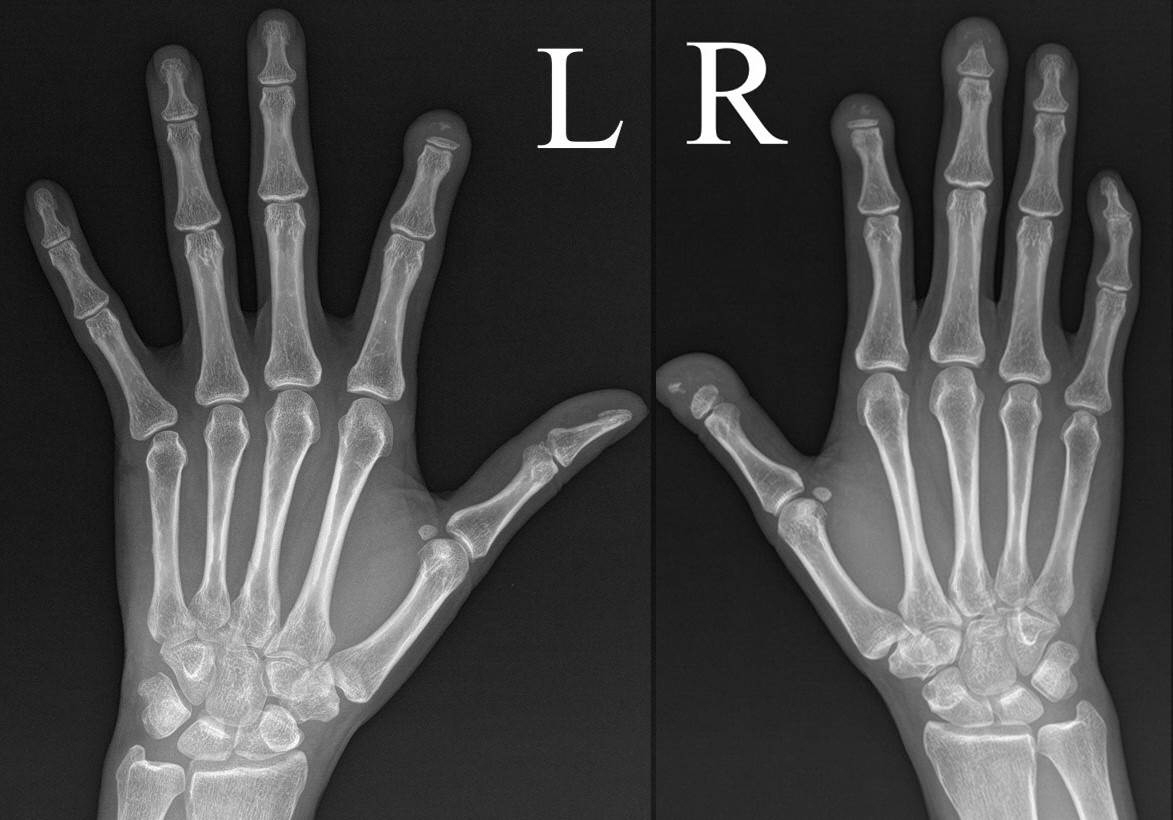
Band acro-osteolysis in a Black woman: a case report and review of the literature
- Affiliations
-
- 1Department of Orthopaedic Surgery, CHA Gumi Medical Center, CHA University, Gumi, Korea
- 2Department of Orthopaedic Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- KMID: 2526650
- DOI: http://doi.org/10.12790/ahm.21.0140
Abstract
- Acro-osteolysis is a bone resorption reaction that progresses slowly in the distal phalanx of the hand and foot and is associated with various diseases. It can be classified as idiopathic or secondary. Although the mechanism of acro-osteolysis has not been fully elucidated, the presence of a chronic ischemic injury appears to have a significant effect, and bone metabolism dysregulation due to the accompanying calcinosis or peripheral neuropathy also appears to contribute. Acro-osteolysis can show various clinical and radiological features, and the differential diagnosis of the underlying etiology is essential. It is a rare and sporadic disease worldwide. The authors experienced a case of acro-osteolysis suspected of idiopathic cause in a Black woman; therefore, we report this case with a literature review.
Keyword
Figure
Reference
-
References
1. Botou A, Bangeas A, Alexiou I, Sakkas LI. Acro-osteolysis. Clin Rheumatol. 2017; 36:9–14.
Article2. Limenis E, Stimec J, Kannu P, Laxer RM. Lost bones: differential diagnosis of acro-osteolysis seen by the pediatric rheumatologist. Pediatr Rheumatol Online J. 2021; 19:113.
Article3. Taylor W, Gladman D, Helliwell P, et al. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum. 2006; 54:2665–73.
Article4. van den Hoogen F, Khanna D, Fransen J, et al. 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Ann Rheum Dis. 2013; 72:1747–55.
Article5. Arana-Ruiz JC, Amezcua-Guerra LM. Acro-osteolysis as an indicator of severity in systemic sclerosis. Reumatol Clin. 2016; 12:263–6.
Article6. Sakchaikul A, Chowchuen P, Foocharoen C, Thammaroj P. Prevalence and clinical association with acro-osteolysis in early systemic sclerosis. Clin Exp Rheumatol. 2021; 39:1093–8.
Article7. Choi WS, Park SY, Ban YS, Kim JH. Acro-osteolysis and calcinosis in patient with scleroderma: a case report. Acta Orthop Traumatol Turc. 2017; 51:88–90.
Article8. Han EJ, Mun JI, An SY, Jung YJ, Kim OH, Chung YS. A case report of hajdu-cheney syndrome. Endocrinol Metab. 2010; 25:152–6.
Article9. Hwang IH, Lim MS, Kim KY, et al. Acroosteolysis of scleroderma associated with a felon. J Korean Orthop Assoc. 2010; 45:88–91.
Article10. Hartzell TL, Makhni EC, Sampson C. Long-term results of periarterial sympathectomy. J Hand Surg Am. 2009; 34:1454–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of acro-osteolysis caused by peripheral neuropathy after minor burn injury
- Effect of Zoledronic Acid on Acro-Osteolysis and Osteoporosis in a Patient with Hajdu-Cheney Syndrome
- Acrogeria
- Pyknodysostosis: report of a rare case with review of literature
- Carpal and tarsal osteolysis: A case report and literature review