Yonsei Med J.
2013 Jan;54(1):131-138. 10.3349/ymj.2013.54.1.131.
Circumferential Resection Margin Involvement in Stage III Rectal Cancer Patients Treated with Curative Resection Followed by Chemoradiotherapy: A Surrogate Marker for Local Recurrence?
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. namkyuk@yuhs.ac
- 2Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1776928
- DOI: http://doi.org/10.3349/ymj.2013.54.1.131
Abstract
- PURPOSE
Circumferential resection margin (CRM) involvement is a well-known predictor for poor prognosis in rectal cancer. However, the significance is controversial in some studies. Accordingly, this study attempted to examine the prognostic impact of CRM involvement in stage III rectal cancer.
MATERIALS AND METHODS
Between January 1990 and December 2007, a total of 449 patients who underwent curative resection followed by complete adjuvant chemoradiotherapy for stage III rectal cancer located within 12 cm from the anal verge were selected. Patients were divided into a CRM-positive group (n=79, 17.6%) and a CRM-negative group (n=370, 82.4%).
RESULTS
With a median follow-up of 56.6 months, recurrent disease was seen in 53.2 and 43.5% of the CRM-positive and CRM-negative group, respectively. CRM involvement was an independent prognostic factor for 5-year systemic recurrence-free survival (HR: 1.5, CI: 1.0-2.2, p=0.017). However, no significant difference was observed for local recurrence rate between the two groups (13.0 and 13.5%, respectively, p=0.677).
CONCLUSION
In this study, local recurrence rate did not differ according to CRM involvement status in stage III rectal cancer patients, although CRM involvement was shown to be an independent poor prognostic factor. Accordingly, validation of the results of this study by further large prospective randomized trials is warranted.
Keyword
MeSH Terms
-
Aged
Biological Markers
Chemoradiotherapy/*methods
Female
Fluorodeoxyglucose F18/pharmacology
Follow-Up Studies
Humans
Lymphatic Metastasis
Magnetic Resonance Imaging
Male
Middle Aged
Neoplasm Metastasis
Neoplasm Recurrence, Local
Neoplasm Staging
Positron-Emission Tomography
Prognosis
Rectal Neoplasms/diagnosis/*surgery/*therapy
Recurrence
Surgical Procedures, Operative
Tomography, X-Ray Computed
Treatment Outcome
Biological Markers
Fluorodeoxyglucose F18
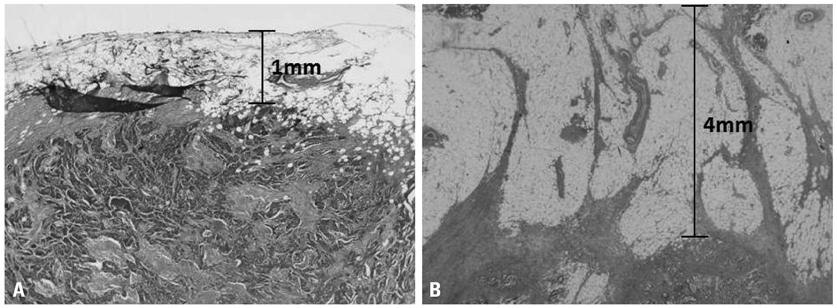
Figure
Cited by 1 articles
-
Machine Learning Model for Predicting Postoperative Survival of Patients with Colorectal Cancer
Mohamed Hosny Osman, Reham Hosny Mohamed, Hossam Mohamed Sarhan, Eun Jung Park, Seung Hyuk Baik, Kang Young Lee, Jeonghyun Kang
Cancer Res Treat. 2022;54(2):517-524. doi: 10.4143/crt.2021.206.
Reference
-
1. Killingback M, Barron P, Dent OF. Local recurrence after curative resection of cancer of the rectum without total mesorectal excision. Dis Colon Rectum. 2001. 44:473–483.
Article2. Yun HR, Lee LJ, Park JH, Cho YK, Cho YB, Lee WY, et al. Local recurrence after curative resection in patients with colon and rectal cancers. Int J Colorectal Dis. 2008. 23:1081–1087.
Article3. Enker WE, Thaler HT, Cranor ML, Polyak T. Total mesorectal excision in the operative treatment of carcinoma of the rectum. J Am Coll Surg. 1995. 181:335–346.4. Cecil TD, Sexton R, Moran BJ, Heald RJ. Total mesorectal excision results in low local recurrence rates in lymph node-positive rectal cancer. Dis Colon Rectum. 2004. 47:1145–1149.
Article5. Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004. 351:1731–1740.
Article6. Hermanek P, Junginger T. The circumferential resection margin in rectal carcinoma surgery. Tech Coloproctol. 2005. 9:193–199.
Article7. Adam IJ, Mohamdee MO, Martin IG, Scott N, Finan PJ, Johnston D, et al. Role of circumferential margin involvement in the local recurrence of rectal cancer. Lancet. 1994. 344:707–711.
Article8. Wibe A, Syse A, Andersen E, Tretli S, Myrvold HE, Søreide O. Norwegian Rectal Cancer Group. Oncological outcomes after total mesorectal excision for cure for cancer of the lower rectum: anterior vs. abdominoperineal resection. Dis Colon Rectum. 2004. 47:48–58.
Article9. Quirke P, Durdey P, Dixon MF, Williams NS. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet. 1986. 2:996–999.10. de Haas-Kock DF, Baeten CG, Jager JJ, Langendijk JA, Schouten LJ, Volovics A, et al. Prognostic significance of radial margins of clearance in rectal cancer. Br J Surg. 1996. 83:781–785.
Article11. Baik SH, Kim NK, Lee YC, Kim H, Lee KY, Sohn SK, et al. Prognostic significance of circumferential resection margin following total mesorectal excision and adjuvant chemoradiotherapy in patients with rectal cancer. Ann Surg Oncol. 2007. 14:462–469.
Article12. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005. 365:1718–1726.
Article13. Hall NR, Finan PJ, al-Jaberi T, Tsang CS, Brown SR, Dixon MF, et al. Circumferential margin involvement after mesorectal excision of rectal cancer with curative intent. Predictor of survival but not local recurrence? Dis Colon Rectum. 1998. 41:979–983.
Article14. Khani M, Smedh K, Kraaz W. Is the circumferential resection margin a predictor of local recurrence after preoperative radiotherapy and optimal surgery for rectal carcinoma? Colorectal Dis. 2007. 9:706–712.
Article15. Kim NK. Anatomic basis of sharp pelvic dissection for curative resection of rectal cancer. Yonsei Med J. 2005. 46:737–749.
Article16. Kim NK, Kim YW, Min BS, Lee KY, Sohn SK, Cho CH. Operative safety and oncologic outcomes of anal sphincter-preserving surgery with mesorectal excision for rectal cancer: 931 consecutive patients treated at a single institution. Ann Surg Oncol. 2009. 16:900–909.
Article17. Kim YW, Kim NK, Min BS, Lee KY, Sohn SK, Cho CH. The influence of the number of retrieved lymph nodes on staging and survival in patients with stage II and III rectal cancer undergoing tumor-specific mesorectal excision. Ann Surg. 2009. 249:965–972.
Article18. Ceelen W, Van Nieuwenhove Y, Pattyn P. Prognostic value of the lymph node ratio in stage III colorectal cancer: a systematic review. Ann Surg Oncol. 2010. 17:2847–2855.
Article19. Brown G, Radcliffe AG, Newcombe RG, Dallimore NS, Bourne MW, Williams GT. Preoperative assessment of prognostic factors in rectal cancer using high-resolution magnetic resonance imaging. Br J Surg. 2003. 90:355–364.
Article20. Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe AG, Dallimore NS, et al. Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology. 2003. 227:371–377.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is a Short Distal Resection Margin of Less than One Centimeter in a Sphincter-saving Resection for Rectal Cancer Oncologically Safe?
- Risk factors of circumferential resection margin involvement in the patients with extraperitoneal rectal cancer
- Surgical issues in locally advanced rectal cancer treated by preoperative chemoradiotherapy
- Long-term Result for Rectal Cancer in Cases of a Curative Resection after Preoperative Chemoradiotherapy
- Oncologic Results according to Operative Method after a Curative Resection for Low Rectal Cancers