Yonsei Med J.
2013 Jan;54(1):34-40. 10.3349/ymj.2013.54.1.34.
Adjunctive Cilostazol versus High Maintenance Dose of Clopidogrel in Patients with Hyporesponsiveness to Chronic Clopidogrel Therapy
- Affiliations
-
- 1Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jyhahn@skku.edu
- 2Department of Laboratory Medicine & Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. suddenbz@skku.edu
- KMID: 1776915
- DOI: http://doi.org/10.3349/ymj.2013.54.1.34
Abstract
- PURPOSE
Whether addition of cilostazol is superior to increasing dose of clopidogrel in patients with hyporesponsiveness to chronic clopidogrel therapy is unknown.
MATERIALS AND METHODS
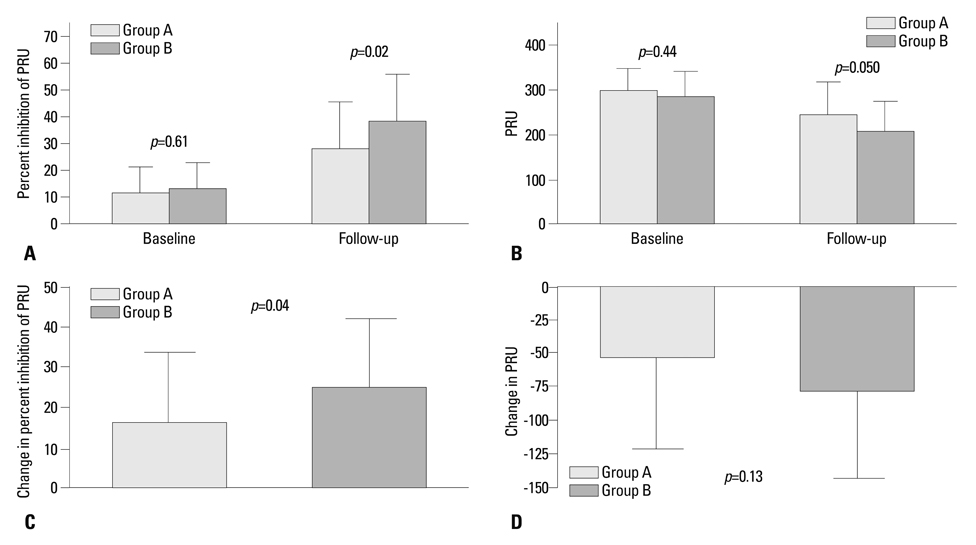
We studied 73 patients with hyporesponsiveness to clopidogrel on standard dual antiplatelet therapy for more than 2 weeks. Clopidogrel hyporesponsiveness was defined as percent inhibition of P2Y12 reaction units (PRU) <30% on VerifyNow P2Y12 assay. Patients were randomly assigned to increased dose of clopidogrel (aspirin 100 mg+clopidogrel 150 mg daily: group A, n=38) or to receiving additional cilostazol (aspirin 100 mg+clopidogrel 75 mg+cilostazol 100 mg bid daily: group B, n=35).
RESULTS
Baseline percent inhibition of PRU and PRU was similar between 2 groups (13.0+/-10.2% versus 11.8+/-9.7%, p=0.61, and 286.3+/-54.7 versus 295.7+/-53.7, p=0.44, respectively). At follow-up, percent inhibition of PRU was higher and PRU was lower significantly in group B than in group A (38.5+/-17.9% versus 28.3+/-16.6%, p=0.02, and 207.3+/-68.2 versus 241.3+/-76.7, p=0.050, respectively). Among those still showing hyporesponsiveness to clopidogrel at follow-up (21 patients in group A, 10 patients in group B), 12 patients completed further crossover study. Compared to the baseline, magnitude of change in percent inhibition of PRU and PRU showed an improved tendency after the crossover (from 2.7+/-8.7% to 15.8+/-18.4%, p=0.08, and from -18.6+/-58.0 to -61.9+/-84.3, p=0.08).
CONCLUSION
Adjunctive cilostazol improved clopidogrel responsiveness better than the higher maintenance dose of clopidogrel in hyporesponsive patients with chronic clopidogrel therapy.
Keyword
MeSH Terms
-
Adult
Aged
Blood Platelets/drug effects
Cross-Over Studies
Drug Administration Schedule
Female
Humans
Male
Middle Aged
Platelet Aggregation Inhibitors/*administration & dosage
Prospective Studies
Receptors, Purinergic P2Y12/metabolism
Tetrazoles/*administration & dosage
Thrombosis/drug therapy
Ticlopidine/administration & dosage/*analogs & derivatives
Time Factors
Treatment Outcome
Platelet Aggregation Inhibitors
Receptors, Purinergic P2Y12
Tetrazoles
Ticlopidine
Figure
Reference
-
1. Serebruany VL, Steinhubl SR, Berger PB, Malinin AI, Bhatt DL, Topol EJ. Variability in platelet responsiveness to clopidogrel among 544 individuals. J Am Coll Cardiol. 2005. 45:246–251.
Article2. Angiolillo DJ, Capranzano P, Goto S, Aslam M, Desai B, Charlton RK, et al. A randomized study assessing the impact of cilostazol on platelet function profiles in patients with diabetes mellitus and coronary artery disease on dual antiplatelet therapy: results of the OPTIMUS-2 study. Eur Heart J. 2008. 29:2202–2211.
Article3. Lee SW, Park SW, Kim YH, Yun SC, Park DW, Lee CW, et al. Comparison of triple versus dual antiplatelet therapy after drug-eluting stent implantation (from the DECLARE-Long trial). Am J Cardiol. 2007. 100:1103–1108.
Article4. Jeong YH, Lee SW, Choi BR, Kim IS, Seo MK, Kwak CH, et al. Randomized comparison of adjunctive cilostazol versus high maintenance dose clopidogrel in patients with high post-treatment platelet reactivity: results of the ACCEL-RESISTANCE (Adjunctive Cilostazol Versus High Maintenance Dose Clopidogrel in Patients With Clopidogrel Resistance) randomized study. J Am Coll Cardiol. 2009. 53:1101–1109.
Article5. Jeong YH, Hwang JY, Kim IS, Park Y, Hwang SJ, Lee SW, et al. Adding cilostazol to dual antiplatelet therapy achieves greater platelet inhibition than high maintenance dose clopidogrel in patients with acute myocardial infarction: results of the adjunctive cilostazol versus high maintenance dose clopidogrel in patients with AMI (ACCEL-AMI) study. Circ Cardiovasc Interv. 2010. 3:17–26.
Article6. Lee K, Lee SW, Lee JW, Kim SY, Youn YJ, Ahn MS, et al. The significance of clopidogrel low-responsiveness on stent thrombosis and cardiac death assessed by the verifynow p(2)y(12) assay in patients with acute coronary syndrome within 6 months after drug-eluting stent implantation. Korean Circ J. 2009. 39:512–518.
Article7. Ono T, Kaikita K, Hokimoto S, Iwashita S, Yamamoto K, Miyazaki Y, et al. Determination of cut-off levels for on-clopidogrel platelet aggregation based on functional CYP2C19 gene variants in patients undergoing elective percutaneous coronary intervention. Thromb Res. 2011. 128:e130–e136.
Article8. Buonamici P, Marcucci R, Migliorini A, Gensini GF, Santini A, Paniccia R, et al. Impact of platelet reactivity after clopidogrel administration on drug-eluting stent thrombosis. J Am Coll Cardiol. 2007. 49:2312–2317.
Article9. Price MJ, Endemann S, Gollapudi RR, Valencia R, Stinis CT, Levisay JP, et al. Prognostic significance of post-clopidogrel platelet reactivity assessed by a point-of-care assay on thrombotic events after drug-eluting stent implantation. Eur Heart J. 2008. 29:992–1000.
Article10. Angiolillo DJ, Shoemaker SB, Desai B, Yuan H, Charlton RK, Bernardo E, et al. Randomized comparison of a high clopidogrel maintenance dose in patients with diabetes mellitus and coronary artery disease: results of the Optimizing Antiplatelet Therapy in Diabetes Mellitus (OPTIMUS) study. Circulation. 2007. 115:708–716.
Article11. Kastrati A, von Beckerath N, Joost A, Pogatsa-Murray G, Gorchakova O, Schömig A. Loading with 600 mg clopidogrel in patients with coronary artery disease with and without chronic clopidogrel therapy. Circulation. 2004. 110:1916–1919.
Article12. von Beckerath N, Kastrati A, Wieczorek A, Pogatsa-Murray G, Sibbing D, Graf I, et al. A double-blind, randomized study on platelet aggregation in patients treated with a daily dose of 150 or 75 mg of clopidogrel for 30 days. Eur Heart J. 2007. 28:1814–1819.
Article13. Wallentin L, Varenhorst C, James S, Erlinge D, Braun OO, Jakubowski JA, et al. Prasugrel achieves greater and faster P2Y12receptor-mediated platelet inhibition than clopidogrel due to more efficient generation of its active metabolite in aspirin-treated patients with coronary artery disease. Eur Heart J. 2008. 29:21–30.
Article14. Mullangi R, Srinivas NR. Clopidogrel: review of bioanalytical methods, pharmacokinetics/pharmacodynamics, and update on recent trends in drug-drug interaction studies. Biomed Chromatogr. 2009. 23:26–41.
Article15. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, Alfonso F, Macaya C, Bass TA, et al. Variability in individual responsiveness to clopidogrel: clinical implications, management, and future perspectives. J Am Coll Cardiol. 2007. 49:1505–1516.16. Dindyal S, Kyriakides C. A review of cilostazol, a phosphodiesterase inhibitor, and its role in preventing both coronary and peripheral arterial restenosis following endovascular therapy. Recent Pat Cardiovasc Drug Discov. 2009. 4:6–14.
Article17. von Beckerath N, Sibbing D, Jawansky S, Braun S, Morath T, Vogt W, et al. Assessment of platelet response to clopidogrel with multiple electrode aggregometry, the VerifyNow P2Y12 analyzer and platelet Vasodilator-Stimulated Phosphoprotein flow cytometry. Blood Coagul Fibrinolysis. 2010. 21:46–52.
Article18. Breet NJ, van Werkum JW, Bouman HJ, Kelder JC, Ruven HJ, Bal ET, et al. Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation. JAMA. 2010. 303:754–762.
Article19. Kim IS, Jeong YH, Park Y, Park KS, Yun SE, Park JR, et al. Platelet inhibition by adjunctive cilostazol versus high maintenance-dose clopidogrel in patients with acute myocardial infarction according to cytochrome P450 2C19 genotype. JACC Cardiovasc Interv. 2011. 4:381–391.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Cilostazol on the Drug-Eluting Stent in Native Coronary Arteries
- A Case of Conjunctival and Periorbital Hemorrhage Spontaneously Occurred in Clopidogrel-treated Patient
- Effects of Cilostazol on Platelet Activation in Coronary Stenting Patients Who Already Treated with Aspirin and Clopidogrel
- Treatment of In-Stent Stenosis Following Flow Diversion of Intracranial Aneurysms with Cilostazol and Clopidogrel
- Clinical Outcomes of Antiplatelets Combined with Statins in Patients with Ischemic Heart Disease