Korean J Gastroenterol.
2010 Dec;56(6):365-372. 10.4166/kjg.2010.56.6.365.
Treatment Efficacy of Clevudine, Entecavir and Lamivudine in Treatment-naive Patients with HBeAg-Positive Chronic Hepatitis B
- Affiliations
-
- 1Department of Gastroenterology, Dong-A University College of Medicine, Busan, Korea. syhan@dau.ac.kr
- KMID: 1775852
- DOI: http://doi.org/10.4166/kjg.2010.56.6.365
Abstract
- BACKGROUND/AIMS
Clevudine is a potent antiviral agent that has demonstrated efficacy in patients with chronic hepatitis B. This study compared the efficacy of clevudine (C), entecavir (E) and lamivudine (L) in treatment-naive patient with HBeAg-positive chronic hepatitis B.
METHODS
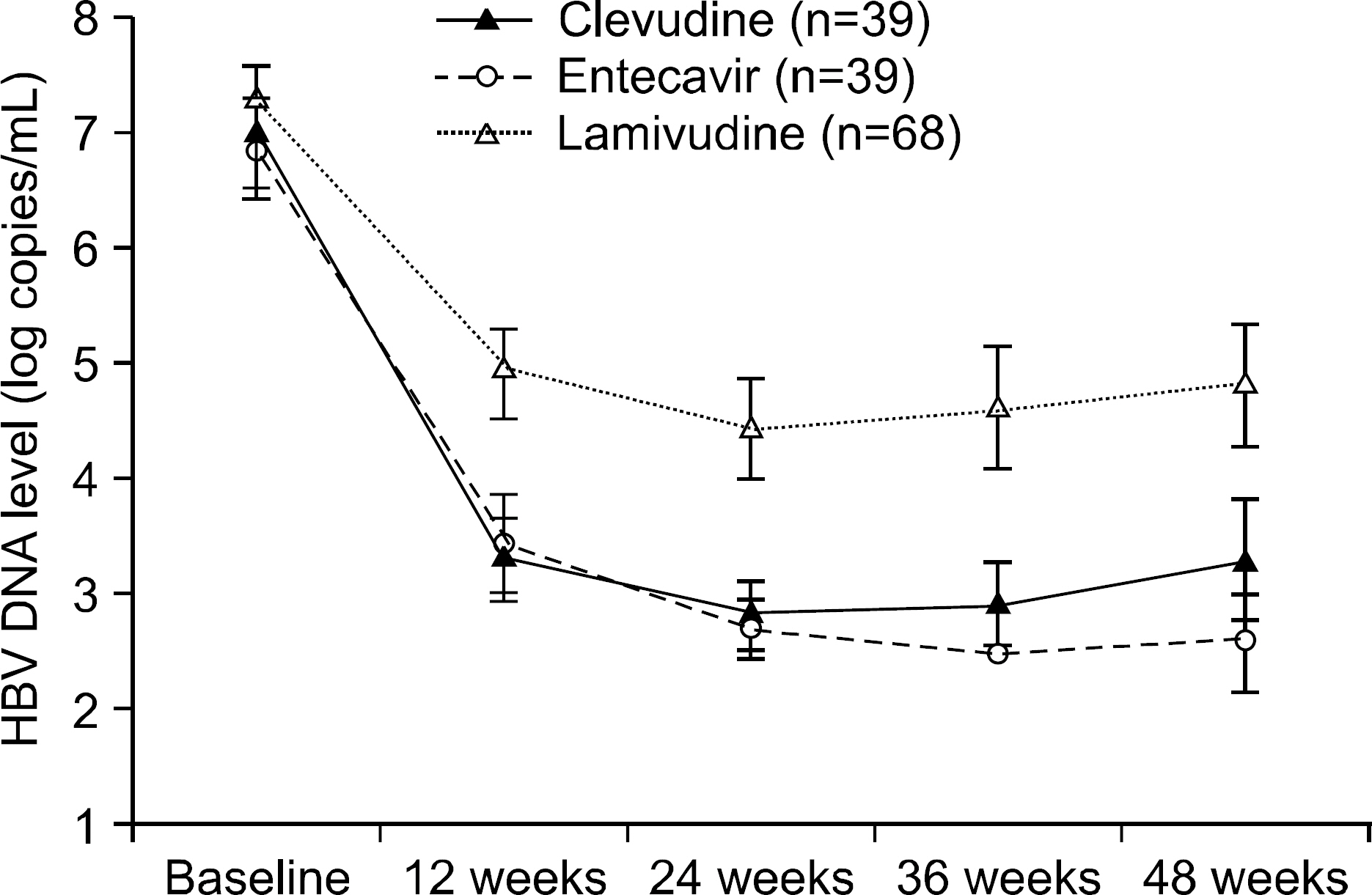
A total of 146 treatment-naive patients with HBeAg-positive chronic hepatitis B received clevudine, entecavir or lamivudine. C group (n=39) received 30 mg of clevudine, E group (n=39) received 0.5 mg of entecavir and L group (n=68) received 100 mg of lamivudine once a day for more than 48 weeks. The efficacy analysis estimated the mean changes of the HBV DNA levels as a virologic response, the normalization of the ALT levels (less than 35 IU/L) as a biochemical response and loss of HBeAg or seroconversion as a serologic response. The serum HBV DNA level was quantified by hybrid capture and real-time PCR assay.
RESULTS
Before the administration of clevudine, entecavir and lamivudine, the mean HBV DNA and ALT levels and the gender and age were well balanced among the three groups (p>0.05). For the virologic response at 48 weeks, the mean changes of the HBV DNA levels from baseline of the C, E and L groups were -3.8+/-2.2, -4.5+/-1.9 and -2.5+/-2.1 log copies/mL. C and E group showed superior antiviral activity compared to that of L group (p<0.0001), but no significant differences in antiviral response were noted between C and E groups. For the biochemical response at 48 weeks, the normalization of the ALT levels (less than 35 IU/L) among the C, E and L groups was 82%, 74% and 71%, respectively (p=0.46). The rates of undetectable serum HBV DNA (less than 300 copies/mL) of the C, E and L groups were 39%, 69% and 27%, respectively (p<0.0001). For the serologic response at 48 weeks, the loss of HBeAg was 13%, 31% and 24% and the seroconversion was 10%, 23% and 17%, respectively. There was no difference of efficacy among the three groups regarding ALT normalization or serologic response (p>0.05). Viral breakthrough in C group was noted at 24 weeks (5%) and 48 weeks (21%), but no biochemical breakthrough was noted. The elevation of the serum CK level was noted in only 1 patient of group C at 48 weeks (2.56%) after therapy. For the patients without or with liver cirrhosis (LC), C and E group showed superior antiviral activity compared to that of the L group, but the antiviral activity was more effective in non- LC group than LC group (p<0.0001 vs p=0.036).
CONCLUSIONS
Clevudine therapy compared with lamivudine for 48 weeks showed significantly potent antiviral efficacy in treatment-naive patients with HBeAg-positive chronic hepatitis B, and especially in the non-LC patients. However, the antiviral efficacy of clevudine was similar to that of entecavir even though taking into account relatively short follow up period and retrospective study.
Keyword
MeSH Terms
-
Adult
Alanine Transaminase/blood
Antiviral Agents/*administration & dosage
Arabinofuranosyluracil/administration & dosage/*analogs & derivatives
DNA, Viral/blood
Drug Administration Schedule
Drug Resistance, Viral
Female
Guanine/administration & dosage/*analogs & derivatives
Hepatitis B e Antigens/*blood
Hepatitis B, Chronic/*drug therapy
Humans
Lamivudine/*administration & dosage
Male
Middle Aged
Retrospective Studies
Treatment Outcome
Figure
Reference
-
1. Cheong JY. Management of chronic hepatitis B in treatment-naive patients. Korean J Gastroenterol. 2008; 51:338–345.2. Iloeje UH, Yang HI, Su J, et al. Predicting cirrhosis risk based on the level of circulating hepatitis B viral load. Gastroenterology. 2006; 130:678–686.
Article3. Chen CJ, Yang HI, Su J, et al. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006; 295:65–73.
Article4. Chen G, Lin WY, Shen FM, Iloeje UH, London WT, Evans AA. Viral load as a predictor of mortality from hepatocellular carcinoma and chronic liver disease in chronic hepatitis B infection. Abstract 477. 40th EASL. April 13-17, 2005. Paris, France.5. Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology. 2007; 45:507–539.
Article6. Mommeja-Marin H, Mondou E, Blum MR, Rousseau F. Serum HBV DNA as a marker of efficacy during therapy for chronic HBV infection: analysis and review of the literature. Hepatology. 2003; 37:1309–1319.
Article7. Di Marco V, Lo Iacono O, Cammà C, et al. The longterm course of chronic hepatitis B. Hepatology. 1999; 30:257–264.
Article8. Dienstag JL, Goldin RD, Heathcote EJ, et al. Histological outcome during longterm lamivudine therapy. Gastroenterology. 2003; 124:105–117.
Article9. Leung NW, Lai CL, Chang TT, et al. Extended lamivudine treatment in patients with chronic hepatitis B enhances hepatitis B e antigen seroconversion rates: results after 3 years of therapy. Hepatology. 2001; 33:1527–1532.
Article10. Dienstag JL, Schiff ER, Wright TL, et al. Lamivudine as initial treatment for chronic hepatitis B in the United States. N Engl J Med. 1999; 341:1256–1263.
Article11. Chang TT, Gish RG, de Man R, et al. A comparison of entecavir and lamivudine for HBeAg-positive chronic hepatitis B. N Engl J Med. 2006; 354:1001–1010.
Article12. Lai CL, Shouval D, Lok AS, et al. Entecavir versus lamivudine for patients with HBeAg-negative chronic hepatitis B. N Engl J Med. 2006; 354:1011–1020.
Article13. Sherman M, Yurdaydin C, Simek H, et al. Entecavir therapy for lamivudine-refractory chronic hepatitis B: improved virologic, biochemical, and serology outcomes through 96 weeks. Hepatology. 2008; 48:99–108.
Article14. Lim SG, Leung N, Hann HW, et al. Clinical trial: a phase II, randomized study evaluating the safety, pharmacokinetics and anti-viral activity of clevudine for 12 weeks in patients with chronic hepatitis B. Aliment Pharmacol Ther. 2008; 27:1282–1292.15. Lee KS, Byun KS, Chung YH, et al. Clevudine therapy for 24 weeks further reduced serum hepatitis B virus DNA levels and increased ALT normalization rates without emergence of viral breakthrough than 12 weeks of clevudine therapy. Intervirology. 2007; 50:296–302.
Article16. Yoo BC, Kim JH, Chung YH, et al. Twenty-four-week clevudine therapy showed potent and sustained antiviral activity in HBeAg-positive chronic hepatitis B. Hepatology. 2007; 45:1172–1178.
Article17. Yoo BC, Kim JH, Kim TH, et al. Clevudine is highly effica-cious in hepatitis B e antigen-negative chronic hepatitis B with durable off-therapy viral suppression. Hepatology. 2007; 46:1041–1048.
Article18. Lee HJ, Eun JR, Lee CH, et al. Longterm clevudine therapy in nucleos(t)idenaïve and lamivudine-experienced patients with hepatitis B virus-related chronic liver diseases. Korean J Hepatol. 2009; 15:179–192.
Article19. Seok JI, Lee DK, Lee CH, et al. Longterm therapy with clevudine for chronic hepatitis B can be associated with myo-pathy characterized by depletion of mitochondrial DNA. Hepatology. 2009; 49:2080–2086.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment Outcomes of Clevudine versus Lamivudine at Week 48 in Naive Patients with HBeAg Positive Chronic Hepatitis B
- Efficacy of New Anti-viral Agent in the Treatment of Chronic Hepatitis B
- Forty-eight weeks treatment with clevudine 30 mg qd versus lamivudine 100 mg qd for chronic hepatitis B infection: a double-blind randomized study
- Effect of Entecavir in Patients Who Lack Lamivudine Resistance after Lamivudine Treatment for Chronic Hepatitis B
- The management and treatment of chronic hepatitis B in Korean children