Korean J Gastroenterol.
2012 Nov;60(5):330-334. 10.4166/kjg.2012.60.5.330.
A Case of Steroid-induced Hyperinfective Strongyloidiasis with Bacterial Meningitis
- Affiliations
-
- 1Department of Internal Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea. kwonjg@cu.ac.kr
- 2Department of Family Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea.
- 3Department of Pathology, Catholic University of Daegu School of Medicine, Daegu, Korea.
- KMID: 1775800
- DOI: http://doi.org/10.4166/kjg.2012.60.5.330
Abstract
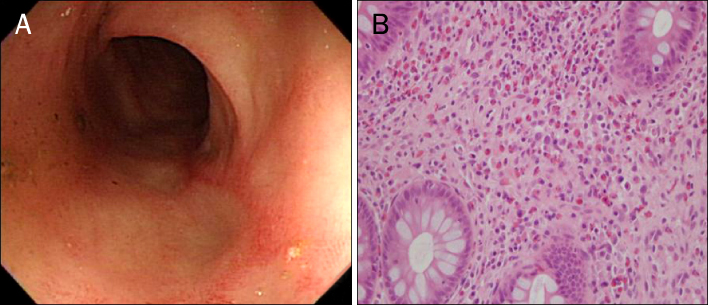
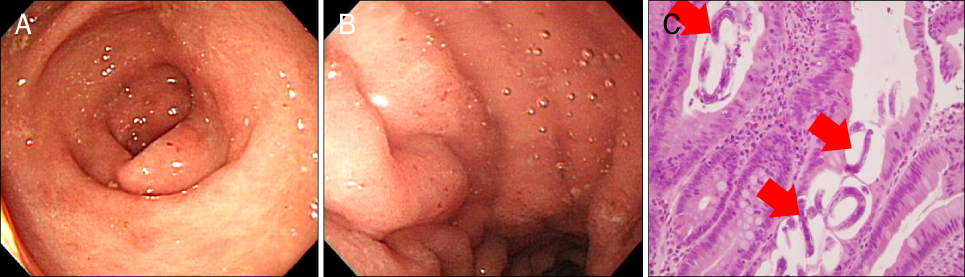
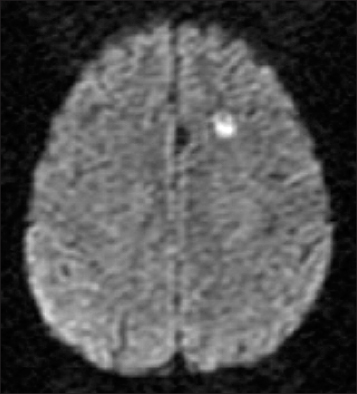
- Strongyloides stercoralis is a soil transmitted intestinal nematode that is endemic in the tropical and subtropical regions. In most individuals who are infected, chronic, usually asymptomatic, gastrointestinal infection persists. But, in immunocompromized hosts or in patients receiving immunosuppressive therapy, autoinfection of S. stercoralis may result in the dissemination of larvae, leading to fatal hyperinfection and increased rate of complications. We report a case of hyperinfective strongyloidiasis with bacterial meningitis in a patient receiving steroid therapy. Strongyloidiasis was diagnosed by the presence of filariform larvae of S. stercoralis in the bronchoalveolar lavage cytology and upper gastrointestinal endoscopic biopsy specimen. Her clinical symptoms had progressively aggravated and developed bacterial meningitis during treatment. She died despite aggressive antibiotic and antihelminthic therapy.
Keyword
MeSH Terms
-
Adrenal Insufficiency/drug therapy
Aged
Animals
Bronchoalveolar Lavage Fluid/parasitology
Endoscopy, Gastrointestinal
Enterococcus faecium/isolation & purification
Female
Humans
Immunocompromised Host
Intestinal Mucosa/pathology
Larva/physiology
Magnetic Resonance Imaging
Meningitis, Bacterial/complications/*diagnosis/microbiology
Steroids/adverse effects/therapeutic use
Strongyloides stercoralis/growth & development/isolation & purification
Strongyloidiasis/complications/*diagnosis/parasitology
Steroids
Figure
Cited by 1 articles
-
A Case of Chronic Strongyloidiasis with Recurrent Hyperinfection
Kuenyoul Park, Min-Sun Kim, Jeonghyun Chang, Eo Jin Kim, Changhoon Yoo, Min Jae Kim, Heungsup Sung, Mi-Na Kim
Lab Med Online. 2019;9(3):171-176. doi: 10.3343/lmo.2019.9.3.171.
Reference
-
1. Genta RM. Global prevalence of strongyloidiasis: critical review with epidemiologic insights into the prevention of disseminated disease. Rev Infect Dis. 1989. 11:755–767.2. Liu LX, Weller PF. Strongyloidiasis and other intestinal nematode infections. Infect Dis Clin North Am. 1993. 7:655–682.3. Kim J, Joo HS, Kim DH, Lim H, Kang YH, Kim MS. A case of gastric strongyloidiasis in a Korean patient. Korean J Parasitol. 2003. 41:63–67.4. Keiser PB, Nutman TB. Strongyloides stercoralis in the immunocompromised population. Clin Microbiol Rev. 2004. 17:208–217.5. Cruz T, Reboucas G, Rocha H. Fatal strongyloidiasis in patients receiving corticosteroids. N Engl J Med. 1966. 275:1093–1096.6. Grove DI. Human strongyloidiasis. Adv Parasitol. 1996. 38:251–309.7. Choi SI, Hong SW, Lee KG. Hyperinfection syndrome with Strongyloides stercoralis: Report of a case. Korean J Pathol. 1989. 23:359–364.8. Siddiqui AA, Berk SL. Diagnosis of strongyloides stercoralis infection. Clin Infect Dis. 2001. 33:1040–1047.9. Koh ES, Kang SB, Lee JH, et al. A case of Strongyloides stercoralis concurrently invading the stomach and colon. Korean J Gastrointest Endosc. 2010. 41:123–127.10. Berk SL, Verghese A, Alvarez S, Hall K, Smith B. Clinical and epidemiologic features of strongyloidiasis. A prospective study in rural Tennessee. Arch Intern Med. 1987. 147:1257–1261.11. Smith JD, Goette DK, Odom RB. Larva currens. Cutaneous strongyloidiasis. Arch Dermatol. 1976. 112:1161–1163.12. Concha R, Harrington W Jr, Rogers AI. Intestinal strongyloidiasis: recognition, management, and determinants of outcome. J Clin Gastroenterol. 2005. 39:203–211.13. Yoon CH, Kim HO, Kim MY, et al. A case of strongyloides stercoralis infection of stomach in association with meningitis. Korean J Med. 1997. 52:550–553.14. Kim HS, Kim YE, Yun EY, et al. A case of fatal hyperinfective strongyloidiasis with acute respiratory failure and intestinal perforation in lung cancer patient. Tuberc Respir Dis. 2010. 68:29–33.15. Lee SH, Ahn SJ, Koh IY, et al. A case of Strongyloidiasis associated with intestinal obstruction in a patient with alcoholic liver disease. Infect Chemother. 2003. 35:467–470.16. Barr JR. Strongyloides stercoralis. Can Med Assoc J. 1978. 118:933–935.17. Marcos LA, Terashima A, Dupont HL, Gotuzzo E. Strongyloides hyperinfection syndrome: an emerging global infectious disease. Trans R Soc Trop Med Hyg. 2008. 102:314–318.18. Gupta S, Jain A, Fanning TV, Couriel DR, Jimenez CA, Eapen GA. An unusual cause of alveolar hemorrhage post hematopoietic stem cell transplantation: a case report. BMC Cancer. 2006. 6:87.19. Link K, Orenstein R. Bacterial complications of Strongyloidiasis: Streptococcus bovis meningitis. South Med J. 1999. 92:728–731.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sweet's Syndrome Associated with Bacterial Meningitis
- A Case of Strongyloides Stercoralis Infection of Stomach in Association with Meningitis
- A Case of Bacterial Meningitis Associated with Cerebral Infarction and Arterial Stenosis-Transcranial Doppler Findings
- A case of chemical meningitis after myelography
- Applying the Bacterial Meningitis Score in Neonates Diagnosed Meningitis: A Single Center Experience