Korean J Radiol.
2007 Oct;8(5):372-381. 10.3348/kjr.2007.8.5.372.
Serial CT Findings of Paragonimus Infested Dogs and the Micro-CT Findings of the Worm Cysts
- Affiliations
-
- 1Department of Radiology and the Institute of Radiation Medicine, Seoul National University College of Medicine, Seoul, Korea. imjg@snu.ac.kr
- 2Seoul National University Hospital, Healthcare Gangnam Center, Seoul, Korea.
- 3Department of Parasitology and Tropical Medicine, Seoul National University Hospital, Seoul, Korea.
- 4Department of Pathology, Seoul National University Hospital, Seoul, Korea.
- KMID: 1734285
- DOI: http://doi.org/10.3348/kjr.2007.8.5.372
Abstract
OBJECTIVE
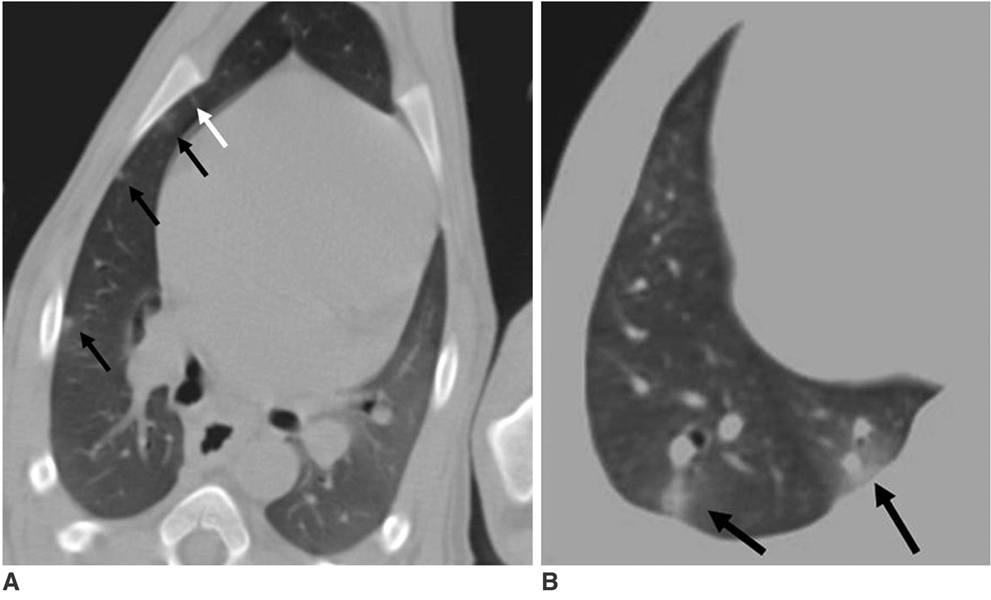
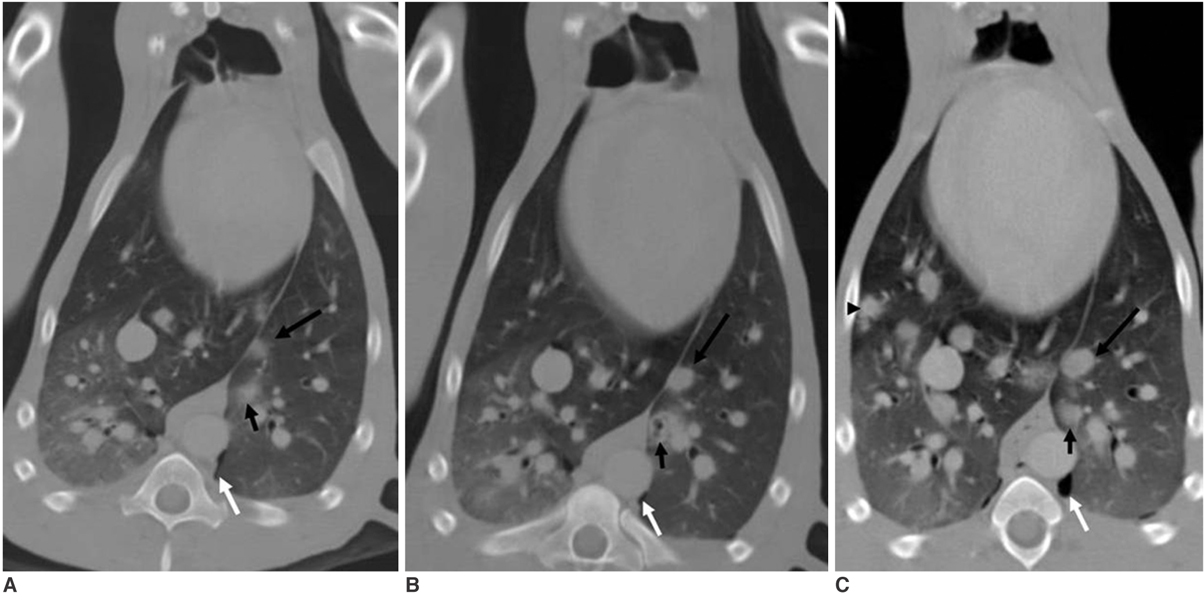
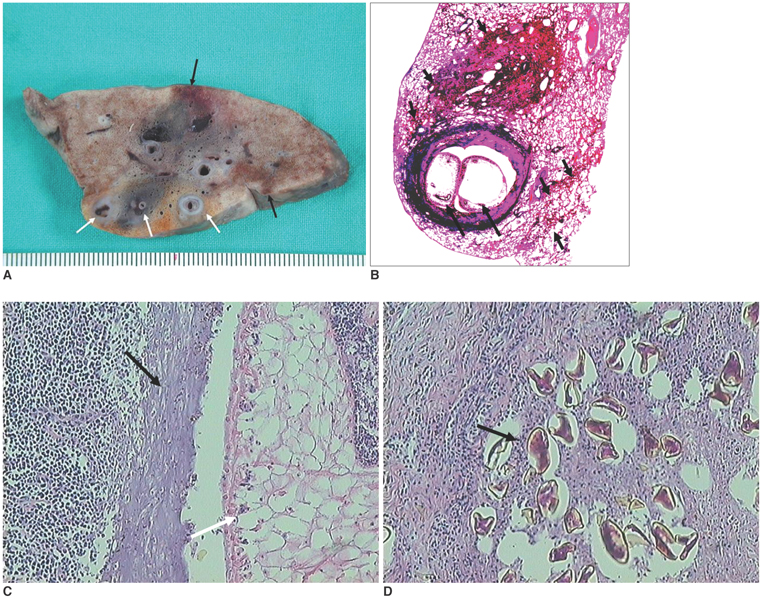
To investigate the serial CT findings of Paragonimus westermani infected dogs and the microscopic structures of the worm cysts using Micro-CT. MATERIALS AND METHODS: This study was approved by the committee on animal research at our institution. Fifteen dogs infected with P. westermani underwent serial contrast-enhanced CT scans at pre-infection, after 10 days of infection, and monthly thereafter until six months for determining the radiologic-pathologic correlation. Three dogs (one dog each time) were sacrificed at 1, 3 and 6 months, respectively. After fixation of the lungs, both multi-detector CT and Micro-CT were performed for examining the worm cysts. RESULTS: The initial findings were pleural effusion and/or subpleural ground-glass opacities or linear opacities at day 10. At day 30, subpleural and peribronchial nodules appeared with hydropneumothorax and abdominal or chest wall air bubbles. Cavitary change and bronchial dilatation began to be seen on CT scan at day 30 and this was mostly seen together with mediastinal lymphadenopathy at day 60. Thereafter, subpleural ground-glass opacities and nodules with or without cavitary changes were persistently observed until day 180. After cavitary change of the nodules, the migratory features of the subpleural or peribronchial nodules were seen on all the serial CT scans. Micro-CT showed that the cyst wall contained dilated interconnected tubular structures, which had communications with the cavity and the adjacent distal bronchus. CONCLUSION: The CT findings of paragonimiasis depend on the migratory stage of the worms. The worm cyst can have numerous interconnected tubular channels within its own wall and these channels have connections with the cavity and the adjacent distal bronchus.
MeSH Terms
-
Animals
Contrast Media/administration & dosage
Cysts/*parasitology/*radiography
Disease Progression
Dogs
Female
Follow-Up Studies
Hydropneumothorax/parasitology
Iohexol/analogs & derivatives/diagnostic use
Lung/parasitology/radiography
Male
Observer Variation
Paragonimiasis/*diagnosis/parasitology
Paragonimus westermani/growth & development/isolation & purification
Pleural Effusion/parasitology
Radiographic Image Enhancement/methods
Time Factors
Tomography, X-Ray Computed/*methods
Figure
Reference
-
1. Sachs R, Albiez EJ, Voelker J. Prevalence of Paragonimus uterobilateralis infection in children in a Liberian village. Trans R Soc Trop Med Hyg. 1986. 80:800–801.2. Yokogawa M. Paragonimus and paragonimiasis. Adv Parasitol. 1969. 7:375–387.3. Sadun EH, Buck AA. Paragonimiasis in South Korea: immunodiagnostic, epidemiologic, clinical, roentgenologic and therapeutic studies. Am J Trop Med Hyg. 1960. 9:562–599.4. Choi DW. Paragonimus and paragonimiasis in Korea. Korean J Parasitol. 1990. 28:Suppl. 79–102.5. Im JG, Whang HY, Kim WS, Han MC, Shim YS, Cho SY. Pleuropulmonary paragonimiasis: radiologic findings in 71 patients. AJR Am J Roentgenol. 1992. 159:39–43.6. Shim YS, Cho SY, Han YC. Pulmonary paragonimiasis: a Korean perspective. Semin Respir Med. 1991. 12:35–45.7. Jeon K, Koh WJ, Kim H, Kwon OJ, Kim TS, Lee KS, et al. Clinical features of recently diagnosed pulmonary paragonimiasis in Korea. Chest. 2005. 128:1423–1430.8. Roque FT, Ludwick RW, Bell JC. Pulmonary paragonimiasis; a review with case reports from Korea and the Philippines. Ann Intern Med. 1953. 38:1206–1221.9. Suwanik R, Harinsuta C. Pulmonary paragonimiasis; an evaluation of roentgen findings in 38 positive sputum patients in an endemic area in Thailand. Am J Roentgenol Radium Ther Nucl Med. 1959. 81:236–244.10. Vélez I, Vélasquez LE, Vélez ID. Morphological description and life cycle of Paragonimus sp. (Trematoda: Troglotrematidae): causal agent of human paragonimiasis in Colombia. J Parasitol. 2003. 89:749–755.11. Nwokolo C. Outbreak of paragonimiasis in Eastern Nigeria. Lancet. 1972. 1:32–33.12. Johnson RJ, Johnson JR. Paragonimiasis in Indochinese refugees. Roentgenographic findings with clinical correlations. Am Rev Respir Dis. 1983. 128:534–538.13. Johnson JR, Falk A, Iber C, Davies S. Paragonimiasis in the United States. A report of nine cases in Hmong immigrants. Chest. 1982. 82:168–171.14. Burton K, Yogev R, London N, Boyer K, Shulman ST. Pulmonary paragonimiasis in Laotian refugee children. Pediatrics. 1982. 70:246–248.15. Collins MS, Phelan A, Kim TC, Pearson RD. Paragonimus westermani: a cause of cavitary lung disease in an Indochinese refugee. South Med J. 1981. 74:1418–1420.16. World Health Organization (WHO). Report of Joint WHO/FAO workshop on foodborne trematode infections in Asia. 2004. 40–41.17. Im JG, Kong Y, Shin YM, Yang SO, Song JG, Han MC, et al. Pulmonary paragonimiasis: clinical and experimental studies. Radiographics. 1993. 13:575–586.18. Kim TS, Han J, Shim SS, Jeon K, Koh WJ, Lee I, et al. Pleuropulmonary paragonimiasis: CT findings in 31 patients. AJR Am J Roentgenol. 2005. 185:616–621.19. Kuroki M, Hatabu H, Nakata H, Hashiguchi N, Shimizu T, Uchino N, et al. High-resolution computed tomography findings of P. westermani. J Thorac Imaging. 2005. 20:210–213.20. Watanabe S, Nakamura Y, Kariatsumari K, Nagata T, Sakata R, Zinnouchi S, et al. Pulmonary paragonimiasis mimicking lung cancer on FDG-PET imaging. Anticancer Res. 2003. 23:3437–3440.21. Diaconita GH, Goldis GH. Investigations on pathomorphology and pathogenesis of pulmonary paragonimiasis. Acta Tuberc Scand. 1964. 44:53–75.22. Lee OR. A histopathologic study of the lungs infected with Paragonimus westermani in the dog. Korean J Parasitol. 1979. 17:19–44. (Korean).23. Mizuki M, Mitoh K, Miyazaki E, Tsuda T. A case of Paragonimiasis westermani with pleural effusion eight months after migrating subcutaneous induration of the abdominal wall. Nihon Kyobu Shikkan Gakkai Zasshi. 1992. 30:1125–1130.24. Choi WY, Jeong SS. A case of paragonimiasis in the abdominal subcutaneous tissue. Korean J Parasitol. 1991. 29:407–409.25. Takemasa H, Saito K, Nakayamada S, Kanazawa T, Tanaka Y. A case of Paragonimiasis westermani complicated with migrating subcutaneous induration and multiple involvements in the liver. Kansenshogaku Zasshi. 2002. 76:594–599.