J Korean Med Assoc.
2004 Mar;47(3):239-244. 10.5124/jkma.2004.47.3.239.
Management of Otitis Media in Children
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Severance Hospital, Korea. dskim6634@yumc.yonsei.ac.kr
- KMID: 1723797
- DOI: http://doi.org/10.5124/jkma.2004.47.3.239
Abstract
- Otitls media is one of the most common diseases during childhood with a peak incidence and prevalence from 6 to 20 months of age. It is the most frequent disease managed with antibiotics in children. The infection typically develops as a result of bacterial contamination through the Eustachian tube in the presence of preexisting inflammation in the middle ear. The optimal method of management remains open to question and is the subject of continuing controversy. Over-diagnosis of the disease and unnecessary prescription of antibiotics for this condition have contributed to the spread of antimicrobial resistance. Thus, the differential diagnosis between acute otitis media and otitis media with effusion is important to determine the management strategy; whether to use antibiotics and which antibiotics to use when necessary. Otitis media may be accompanied by a variable degree of conductive hearing loss. Both infectious and noninfectious complications of otitis media may result in significant morbidity and complications, including acute and chronic mastoiditis, petrositis, and intracranial infection.
MeSH Terms
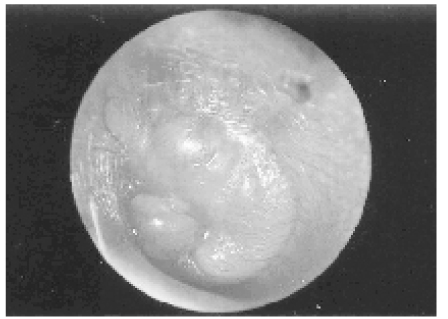
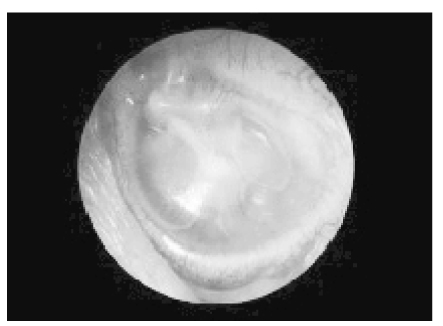
Figure
Reference
-
1. Rutka J, Lekagul S. No therapy:use, abuse, efficacy, and morbidity-the European versus the Third-World experience. J Otolaryngol. 1998. 27:Suppl 2. 43–48.2. Gates GA. Cummings CW, Fredrickson JM, Harker LA, Krause CJ, Richardson MA, Scculler DE, editors. Acute otitis media and otitis media with effusion. Otolaryngology Head & Neck Surgery. 1998. 3rd ed. Mosby Co;461–477.3. Rosenfeld RM. An evidence-based approach to treating otitis media. Pediatr Clin North Am. 1996. 43:1165–1181.
Article4. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ. 2001. 322:336–342.
Article5. Froom J, Culpepper L, Jacobs M, DeMelker RA, Green LA, Heeren T, et al. Antimicrobials for acute otitis media:A review from the International Primary Care Network. BMJ. 1997. 315:98–102.
Article6. Dowell SF, Butler JC, Giebink GS, Jacobs MR, Jernigan D, Schwartz B, et al. Acute otitis media:management and surveillance in an era of pneumococcal resistnace-a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working Group. Pediatr Infect Dis J. 1999. 18:1–9.
Article7. Bitnun A, Allen UD. Medical therapy of otitis media: use, abuse, efficacy, and morbidity. J Otolaryngol. 1998. 27:Suppl 2. 26–36.8. Williams RL, Chalmers TC, Stange KC, Chalmers FT, Bowlin SJ. Use of antibiotics in preventing recurrent otitis media and in treating otitis media with effusion:a meta-analytic attempt to resolve the brouhaha. JAMA. 1993. 270:1344–1351.
Article9. Alho OP, Läärä E, Oja H. What is the natural history of recurrent acute otitis media in infancy? J Fam Pract. 1996. 43:258–264.10. Rosenfeld RM, Vertrees JE, Carr J, Cipolle RJ, Uden DL, Canafax DM, et al. Clinical efficacy of antimicrobial drugs for acute otitis media:meta-analysis of 5400 children from thirty-three randomized trials. J Pediatr. 1994. 124:355–367.
Article11. Schwartz RH, Rosenberg WJ, Schwartz DM. Office myringotomy for acute otitis media:its value in preventing middle ear effusion. Laryngoscope. 1981. 91:616–619.
Article12. American Academy of Pediatrics The Otitis Media Guideline Panel. Managing otitis media with effusion in young children. Pediatrics. 1994. 94(5):766–773.