J Korean Med Assoc.
2015 Jul;58(7):635-644. 10.5124/jkma.2015.58.7.635.
The diagnosis and management of otitis media in children
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University College of Medicine, Chunchen, Korea. hjk1000@hallym.ac.kr
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea.
- KMID: 2064920
- DOI: http://doi.org/10.5124/jkma.2015.58.7.635
Abstract
- Otitis media is one of the most common bacterial infectious diseases in children and the most common indication for the prescription of antibiotics in Korea. Otitis media, including acute otitis media (AOM) and otitis media with effusion (OME), is also one of the most common reasons for an illness-related visit to a primary care clinician. The first step in management decisions regarding otitis media must focus on accurate diagnosis to distinguish normal from AOM or OME. In 2010, the Korean Otologic Society published the first version of a set of evidence-based clinical practice guidelines for pediatric otitis media. In 2014, revised clinical practice guidelines were published for otitis media that applied to children under 15 years of age. The guidelines addressed the diagnosis and management of otitis media as well as pain management, choice of antibiotics, and methods for prevention. These guidelines recognized that many episodes of otitis media will resolve on their own without antimicrobial therapy; therefore, one of the recommendations for the initial treatment of otitis media in specified situations is watchful waiting without antibacterial therapy. This study introduces excerpts of the guidelines for the diagnosis and management of otitis media in children. We then briefly discuss the current knowledge about AOM and OME and address the new AOM and OME guidelines point by point. It is important to remember that the actual management of patients with otitis media should depend on the physician's clinical judgment, the symptoms of the individual child, other underlying medical conditions, ready access to adequate follow-up care, and other features.
MeSH Terms
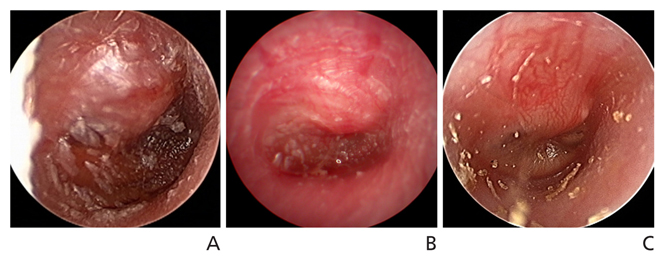
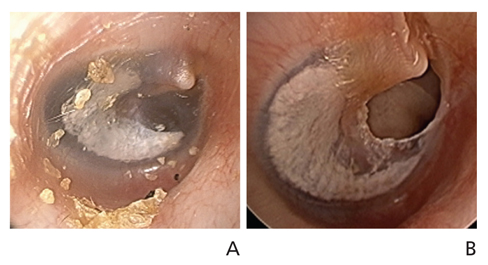
Figure
Reference
-
1. Teele DW, Klein JO, Rosner B. Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective, cohort study. J Infect Dis. 1989; 160:83–94.
Article2. Kim CS, Jung HW, Yoo KY. Prevalence of otitis media and allied diseases in Korea: results of a nation-wide survey, 1991. J Korean Med Sci. 1993; 8:34–40.
Article3. Korean Otologic Society. Korean clinical practice guideline: otitis media in children 2010 [Internet]. Seoul: Korean Medical Guideline Information Center;2010. cited 2015 Jul 2. Available from: http://guideline.or.kr/bbs/guideline.php.4. Korean Otologic Society. Korean clinical practice guideline: otitis media in children 2014 [Internet]. Seoul: Korean Medical Guideline Information Center;2014. cited 2015 Jul 2. Available from: http://guideline.or.kr/bbs/guideline.php.5. American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004; 113:1451–1465.6. Lieberthal AS, Carroll AE, Chonmaitree T, Ganiats TG, Hoberman A, Jackson MA, Joffe MD, Miller DT, Rosenfeld RM, Sevilla XD, Schwartz RH, Thomas PA, Tunkel DE. The diagnosis and management of acute otitis media. Pediatrics. 2013; 131:e964–e999.
Article7. Japan Otological Society. Japan Society for Pediatric Otorhinolaryngology. Japan Society for Infectious Diseases in Otolaryngology. 2006 Clinical practice guideline for diagnosis and management of acute otitis media in children. Tokyo: Kanehara Shuppan;2006.8. Japan Otological Society. Japan Society for Pediatric Otorhinolaryngology. Japan Society for Infectious Diseases in Otolaryngology. 2009 Clinical practice guideline for diagnosis and management of acute otitis media in children. Tokyo: Kanehara Shuppan;2009.9. Rosenfeld RM, Culpepper L, Doyle KJ, Grundfast KM, Hoberman A, Kenna MA, Lieberthal AS, Mahoney M, Wahl RA, Woods CR Jr, Yawn B. American Academy of Pediatrics Subcommittee on Otitis Media with Effusion. American Academy of Family Physicians. American Academy of Otolaryngology Head and Neck Surgery. Clinical practice guideline: otitis media with effusion. Otolaryngol Head Neck Surg. 2004; 130:5 Suppl. S95–S118.
Article10. National Collaborating Centre for Women's and Children's Health. Surgical management of otitis media with effusion in children. London: National Institute for Health and Clinical Excellence;2008.11. Marchisio P, Bellussi L, Di Mauro G, Doria M, Felisati G, Longhi R, Novelli A, Speciale A, Mansi N, Principi N. Acute otitis media: from diagnosis to prevention. Summary of the Italian guideline. Int J Pediatr Otorhinolaryngol. 2010; 74:1209–1216.
Article12. Thomas CL, Simpson S, Butler CC, van der Voort JH. Oral or topical nasal steroids for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst Rev. 2006; (3):CD001935.
Article13. Pichichero ME, Doern GV, Kuti JL, Nicolau DP. Probability of achieving requisite pharmacodynamic exposure for oral beta-lactam regimens against Haemophilus influenzae in children. Paediatr Drugs. 2008; 10:391–397.
Article14. Venekamp RP, Sanders S, Glasziou PP, Del Mar CB, Rovers MM. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2013; 1:CD000219.
Article15. Tahtinen PA, Laine MK, Huovinen P, Jalava J, Ruuskanen O, Ruohola A. A placebo-controlled trial of antimicrobial treatment for acute otitis media. N Engl J Med. 2011; 364:116–126.
Article16. Hoberman A, Paradise JL, Rockette HE, Shaikh N, Wald ER, Kearney DH, Colborn DK, Kurs-Lasky M, Bhatnagar S, Haralam MA, Zoffel LM, Jenkins C, Pope MA, Balentine TL, Barbadora KA. Treatment of acute otitis media in children under 2 years of age. N Engl J Med. 2011; 364:105–115.
Article17. Asher E, Dagan R, Greenberg D, Givon-Lavi N, Libson S, Porat N, Leiberman A, Leibovitz E. Persistence of pathogens despite clinical improvement in antibiotic-treated acute otitis media is associated with clinical and bacteriologic relapse. Pediatr Infect Dis J. 2008; 27:296–301.
Article18. Griffin GH, Flynn C, Bailey RE, Schultz JK. Antihistamines and/or decongestants for otitis media with effusion (OME) in children. Cochrane Database Syst Rev. 2006; (4):CD003423.
Article19. Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Rockette HE, Pitcairn DL, Smith CG, Colborn DK, Bernard BS, Kurs-Lasky M, Janosky JE, Sabo DL, O'Connor RE, Pelham WE Jr. Tympanostomy tubes and developmental outcomes at 9 to 11 years of age. N Engl J Med. 2007; 356:248–261.
Article