Korean Circ J.
2013 Jan;43(1):29-37. 10.4070/kcj.2013.43.1.29.
Characteristics and Outcomes of Atrial Tachycardia Originating from the Sinus Venosus during Catheter Ablation of Atrial Fibrillation
- Affiliations
-
- 1Division of Cardiology, Korea University College of Medicine, Seoul, Korea. yhkmd@unitel.co.kr
- KMID: 1722998
- DOI: http://doi.org/10.4070/kcj.2013.43.1.29
Abstract
- BACKGROUND AND OBJECTIVES
The sinus venosus (SV) is not a well known source of atrial tachycardia (AT), but it can harbor AT during catheter ablation of atrial fibrillation (AF).
SUBJECTS AND METHODS
A total of 1223 patients who underwent catheter ablation for AF were reviewed. Electrophysiological and electrocardiographic characteristics and outcomes after catheter ablation of AT originating from the SV were investigated.
RESULTS
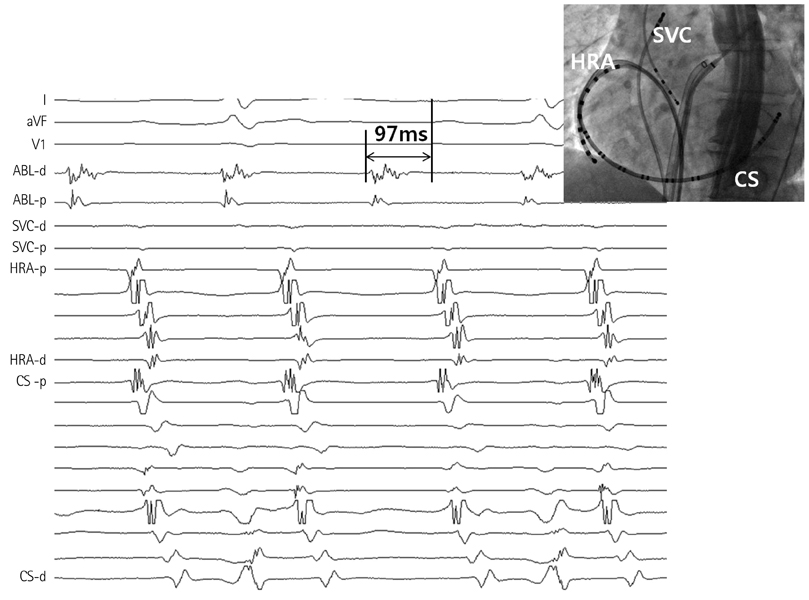
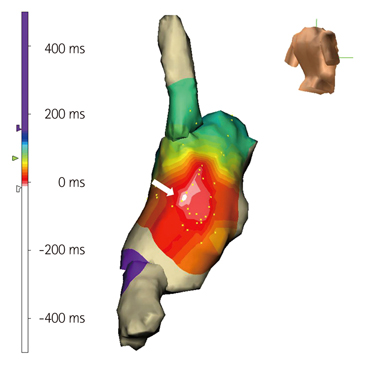
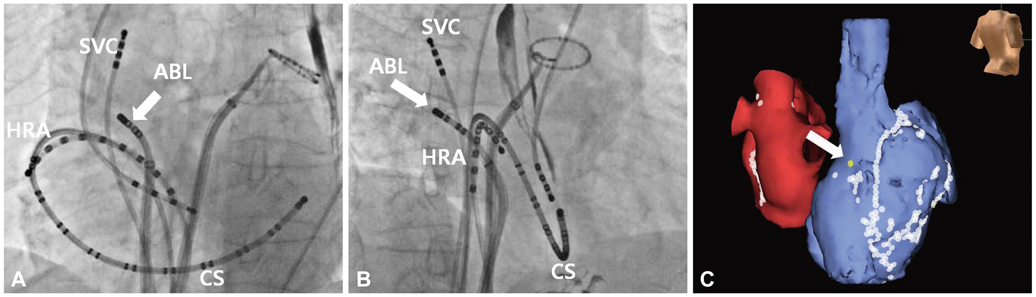
Ten patients (0.82%) demonstrated AT from the SV (7 males, 53.9+/-16.0 years, 6 persistent) during ablation of AF. The mean cycle length was 281+/-73 ms. After pulmonary vein isolation and left atrial ablation, AF converted to AT from the SV during right atrial ablation in 2 patients, by rapid atrial pacing after AF termination in 7 patients, and during isoproterenol infusion in 1 patient. Positive P-waves in inferior leads were shown in most patients (90%). The activation sequence of AT was from proximal to distal in the superior vena cava and high to low in the right atrium, which was similar to that of AT from crista terminalis. Fragmented double potentials were recorded during sinus, and a second discrete potential preceded the onset of P wave by 80+/-37 ms during AT. Using 4.4+/-2.7 radiofrequency focal applications, ATs were terminated and became no longer inducible in all. After ablation procedure, two patients showed transient right phrenic nerve palsy. After 19.9+/-14.8 months, all but 1 patient were free of atrial tachyarrhythmia without complications.
CONCLUSION
The AT which develops during AF ablation is rarely originated from SV, and its electrophysiologic characteristics may be helpful in guiding effective focal ablation.
MeSH Terms
Figure
Reference
-
1. Mesas CE, Pappone C, Lang CC, et al. Left atrial tachycardia after circumferential pulmonary vein ablation for atrial fibrillation: electroanatomic characterization and treatment. J Am Coll Cardiol. 2004. 44:1071–1079.2. Chugh A, Oral H, Lemola K, et al. Prevalence, mechanisms, and clinical significance of macroreentrant atrial tachycardia during and following left atrial ablation for atrial fibrillation. Heart Rhythm. 2005. 2:464–471.3. Chae S, Oral H, Good E, et al. Atrial tachycardia after circumferential pulmonary vein ablation of atrial fibrillation: mechanistic insights, results of catheter ablation, and risk factors for recurrence. J Am Coll Cardiol. 2007. 50:1781–1787.4. Scherr D, Dalal D, Cheema A, et al. Automated detection and characterization of complex fractionated atrial electrograms in human left atrium during atrial fibrillation. Heart Rhythm. 2007. 4:1013–1020.5. Saoudi N, Cosío F, Waldo A, et al. A classification of atrial flutter and regular atrial tachycardia according to electrophysiological mechanisms and anatomical bases; a Statement from a Joint Expert Group from The Working Group of Arrhythmias of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 2001. 22:1162–1182.6. Mohamed U, Skanes AC, Gula LJ, et al. A novel pacing maneuver to localize focal atrial tachycardia. J Cardiovasc Electrophysiol. 2007. 18:1–6.7. Jaïs P, Hocini M, Sanders P, et al. Long-term evaluation of atrial fibrillation ablation guided by noninducibility. Heart Rhythm. 2006. 3:140–145.8. Calkins H, Brugada J, Packer DL, et al. HRS/EHRA/ECAS expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2007. 4:816–861.9. Nam GB, Jin ES, Choi H, et al. Mechanism of regular atrial tachyarrhythmias during combined pulomonary vein isolation and complex fractionated electrogram ablation in patients with atrial fibrillation. Circ J. 2010. 74:434–441.10. Rostock T, Drewitz I, Steven D, et al. Characterization, mapping, and catheter ablation of recurrent atrial tachycardias after stepwise ablation of long-lasting persistent atrial fibrillation. Circ Arrhythm Electrophysiol. 2010. 3:160–169.11. Satomi K. Electrophysiological characteristics of atrial tachycardia after pulmonary vein isolation of atrial fibrillation. Circ J. 2010. 74:1051–1058.12. Haïssaguerre M, Hocini M, Sanders P, et al. Catheter ablation of longlasting persistent atrial fibrillation: clinical outcome and mechanisms of subsequent arrhythmias. J Cardiovasc Electrophysiol. 2005. 16:1138–1147.13. Gonzalez MD, Erga KS, Rivera J, et al. Rate-dependent block in the sinus venosa of the swine heart during transverse right atrial activation: correlation between electrophysiologic and anatomic findings. J Cardiovasc Electrophysiol. 2005. 16:193–200.14. Harada M, Osaka T, Yokoyama E, Takemoto Y, Ito A, Kodama I. Action potential characteristics in the sinus venosa of patients with and without atrial flutter. Circ J. 2009. 73:647–653.15. Lin YJ, Higa S, Tai CT, et al. Role of the right atrial substrate in different types of atrial arrhythmias. Heart Rhythm. 2009. 6:592–598.16. Jaïs P, Matsuo S, Knecht S, et al. A deductive mapping strategy for atrial tachycardia following atrial fibrillation ablation: importance of localized reentry. J Cardiovasc Electrophysiol. 2009. 20:480–491.17. Kistler PM, Roberts-Thomson KC, Haqqani HM, et al. P-wave morphology in focal atrial tachycardia: development of an algorithm to predict the anatomic site of origin. J Am Coll Cardiol. 2006. 48:1010–1017.18. Tang CW, Scheinman MM, Van Hare GF, et al. Use of P wave configuration during atrial tachycardia to predict site of origin. J Am Coll Cardiol. 1995. 26:1315–1324.19. Kistler PM, Kalman JM. Locating focal atrial tachycardias from P-wave morphology. Heart Rhythm. 2005. 2:561–564.20. Qian ZY, Hou XF, Xu DJ, et al. An algorithm to predict the site of origin of focal atrial tachycardia. Pacing Clin Electrophysiol. 2011. 34:414–421.21. Sacher F, Monahan KH, Thomas SP, et al. Phrenic nerve injury after atrial fibrillation catheter ablation: characterization and outcome in a multicenter study. J Am Coll Cardiol. 2006. 47:2498–2503.22. Sánchez-Quintana D, Cabrera JA, Climent V, Farré J, Weiglein A, Ho SY. How close are the phrenic nerves to cardiac structures? Implications for cardiac interventionalists. J Cardiovasc Electrophysiol. 2005. 16:309–313.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Catheter Ablation of Atrial Tachycardia Originating from the Non-coronary Aortic Sinus
- Atrial Tachycardia Originating from the Aortomitral Junction
- Catheter ablation for treatment of tachyarrhythmia
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation
- A case of sinus node dysfunction and atrial tachycardia after the excision of a left atrial myxoma