Korean J Gastroenterol.
2012 Jul;60(1):13-18. 10.4166/kjg.2012.60.1.13.
Incidence and Risk Factors of Irritable Bowel Syndrome in Community Subjects with Culture-proven Bacterial Gastroenteritis
- Affiliations
-
- 1Epidemic Intelligence Service, Division of Public Health Policy, Gyeonggi Provincial Office, Suwon, Korea.
- 2Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. dhljohn@yahoo.co.kr
- KMID: 1718461
- DOI: http://doi.org/10.4166/kjg.2012.60.1.13
Abstract
- BACKGROUND/AIMS
The aim of this study was to investigate the incidence and risk factors of irritable bowel syndrome (IBS) in community subjects with culture-proven bacterial gastroenteritis.
METHODS
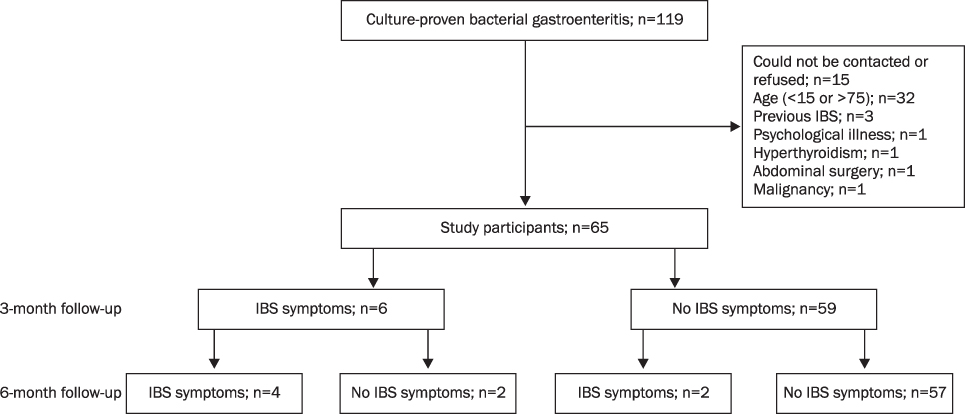
This was a prospective, community-based, cohort study, which followed patients with a recent history of culture-proven bacterial gastroenteritis. IBS was diagnosed with the use of the Rome II criteria at 3 and 6 months after bacterial dysentery.
RESULTS
Sixty five cases were included and completed the 6 month follow-up. Thirty four cases (52.3%) were female. Salmonella was the pathogen most frequently identified and seen in 41 patients (63.1%). The cumulative incidence of IBS among patients with microbiologically proven bacterial gastroenteritis within a community was 9.2% and 12.3% at 3 and 6 months of follow-up, respectively. The duration of initial diarrhea (> or =7 days) was associated with an increased risk for the development of IBS (aOR, 14.50 [95% CI, 1.38-152.72]; p=0.022).
CONCLUSIONS
Our study suggests that the incidence of IBS among patients with culture-proven bacterial gastroenteritis within a community is similar to that reported among Western populations. A large, prospective study is encouraged to confirm our results and to evaluate the influence of the microbial species on the epidemiology of IBS in Asian populations.
MeSH Terms
-
Adolescent
Adult
Aged
Cohort Studies
Diarrhea/complications
Dysentery/complications
Female
Follow-Up Studies
Gastroenteritis/*complications/epidemiology/microbiology
Humans
Incidence
Irritable Bowel Syndrome/*diagnosis/epidemiology/etiology
Male
Middle Aged
Odds Ratio
Prospective Studies
Risk Factors
Salmonella/isolation & purification
Shigella/isolation & purification
Young Adult
Figure
Cited by 1 articles
-
Guideline for the Antibiotic Use in Acute Gastroenteritis
Youn Jeong Kim, Ki-Ho Park, Dong-Ah Park, Joonhong Park, Byoung Wook Bang, Seung Soon Lee, Eun Jung Lee, Hyo-Jin Lee, Sung Kwan Hong, Yang Ree Kim
Infect Chemother. 2019;51(2):217-243. doi: 10.3947/ic.2019.51.2.217.
Reference
-
1. Thompson WG, Longstreth GF, Drossman DA, et al. Functional bowel disorders and functional abdominal pain. Gut. 1999. 45:Suppl 2. II43–II47.2. Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006. 130:1377–1390.3. Swain MG, Blennerhassett PA, Collins SM. Impaired sympathetic nerve function in the inflamed rat intestine. Gastroenterology. 1991. 100:675–682.4. Dunlop SP, Jenkins D, Neal KR, Spiller RC. Relative importance of enterochromaffin cell hyperplasia, anxiety, and depression in postinfectious IBS. Gastroenterology. 2003. 125:1651–1659.5. Spiller RC, Jenkins D, Thornley JP, et al. Increased rectal mucosal enteroendocrine cells, T lymphocytes, and increased gut permeability following acute Campylobacter enteritis and in post-dysenteric irritable bowel syndrome. Gut. 2000. 47:804–811.6. Gwee KA, Collins SM, Read NW, et al. Increased rectal mucosal expression of interleukin 1beta in recently acquired post-infectious irritable bowel syndrome. Gut. 2003. 52:523–526.7. Wang LH, Fang XC, Pan GZ. Bacillary dysentery as a causative factor of irritable bowel syndrome and its pathogenesis. Gut. 2004. 53:1096–1101.8. Rodríguez LA, Ruigómez A. Increased risk of irritable bowel syndrome after bacterial gastroenteritis: cohort study. BMJ. 1999. 318:565–566.9. Parry SD, Stansfield R, Jelley D, et al. Does bacterial gastroenteritis predispose people to functional gastrointestinal disorders? A prospective, community-based, case-control study. Am J Gastroenterol. 2003. 98:1970–1975.10. Thabane M, Kottachchi DT, Marshall JK. Systematic review and meta-analysis: The incidence and prognosis of post-infectious irritable bowel syndrome. Aliment Pharmacol Ther. 2007. 26:535–544.11. Spiller R, Garsed K. Postinfectious irritable bowel syndrome. Gastroenterology. 2009. 136:1979–1988.12. Stewart GT. Post-dysenteric colitis. Br Med J. 1950. 1:405–409.13. Neal KR, Hebden J, Spiller R. Prevalence of gastrointestinal symptoms six months after bacterial gastroenteritis and risk factors for development of the irritable bowel syndrome: postal survey of patients. BMJ. 1997. 314:779–782.14. Ji S, Park H, Lee D, Song YK, Choi JP, Lee SI. Post-infectious irritable bowel syndrome in patients with Shigella infection. J Gastroenterol Hepatol. 2005. 20:381–386.15. Marshall JK, Thabane M, Garg AX, et al. Incidence and epidemiology of irritable bowel syndrome after a large waterborne outbreak of bacterial dysentery. Gastroenterology. 2006. 131:445–450.16. Borgaonkar MR, Ford DC, Marshall JK, Churchill E, Collins SM. The incidence of irritable bowel syndrome among community subjects with previous acute enteric infection. Dig Dis Sci. 2006. 51:1026–1032.17. Parry SD, Barton JR, Welfare MR. Is lactose intolerance implicated in the development of post-infectious irritable bowel syndrome or functional diarrhoea in previously asymptomatic people? Eur J Gastroenterol Hepatol. 2002. 14:1225–1230.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Development of Irritable Bowel Syndrome after Shigella Infection: 3 Year Follow-up Study
- Post-infectious Irritable Bowel Syndrome in the Community: A Prospective Cohort Study
- Estimating the Contribution of Acute Gastroenteritis to the Overall Prevalence of Irritable Bowel Syndrome
- Irritable bowel syndrome
- Prevalence and Risk Factors of Irritable Bowel Syndrome in Asia