Korean J Gastroenterol.
2011 Aug;58(2):93-99. 10.4166/kjg.2011.58.2.93.
Lack of Radiation Protection for Endoscopists Performing Endoscopic Retrograde Cholangiopancreatography
- Affiliations
-
- 1Committee Established for ERCP Guidelines on Radiological Protection, Korean Society of Pancreatobiliary Disease.
- 2Department of Internal Medicine, Eulji University Eulji-General Hospital, Seoul, Korea.
- 3Department of Internal Medicine, Sungkyunkwan University College of Medicine, Samsung Medical Center, Seoul, Korea.
- 4Department of Internal Medicine, Korea University Medical Center, Guro-Hospital, Seoul, Korea.
- 5Department of Internal Medicine, The Research Institute of Clinical Medicine, Chonbuk National University Medical School, Jeonju, Korea. solee@chonbuk.ac.kr
- KMID: 1718416
- DOI: http://doi.org/10.4166/kjg.2011.58.2.93
Abstract
- BACKGROUND/AIMS
ERCP using fluoroscopy should be practiced with an adequate radiation protection. However, the awareness of gastrointestinal endoscopists to radiation protection was considered insufficient. In Korea, a country with a rapid increase the number of ERCP procedures, there is no data about radiation protection practices for gastrointestinal endoscopists. The purpose of this study was to investigate current clinical practices and the awareness on radiation protection in ERCP performing physicians in Korea.
METHODS
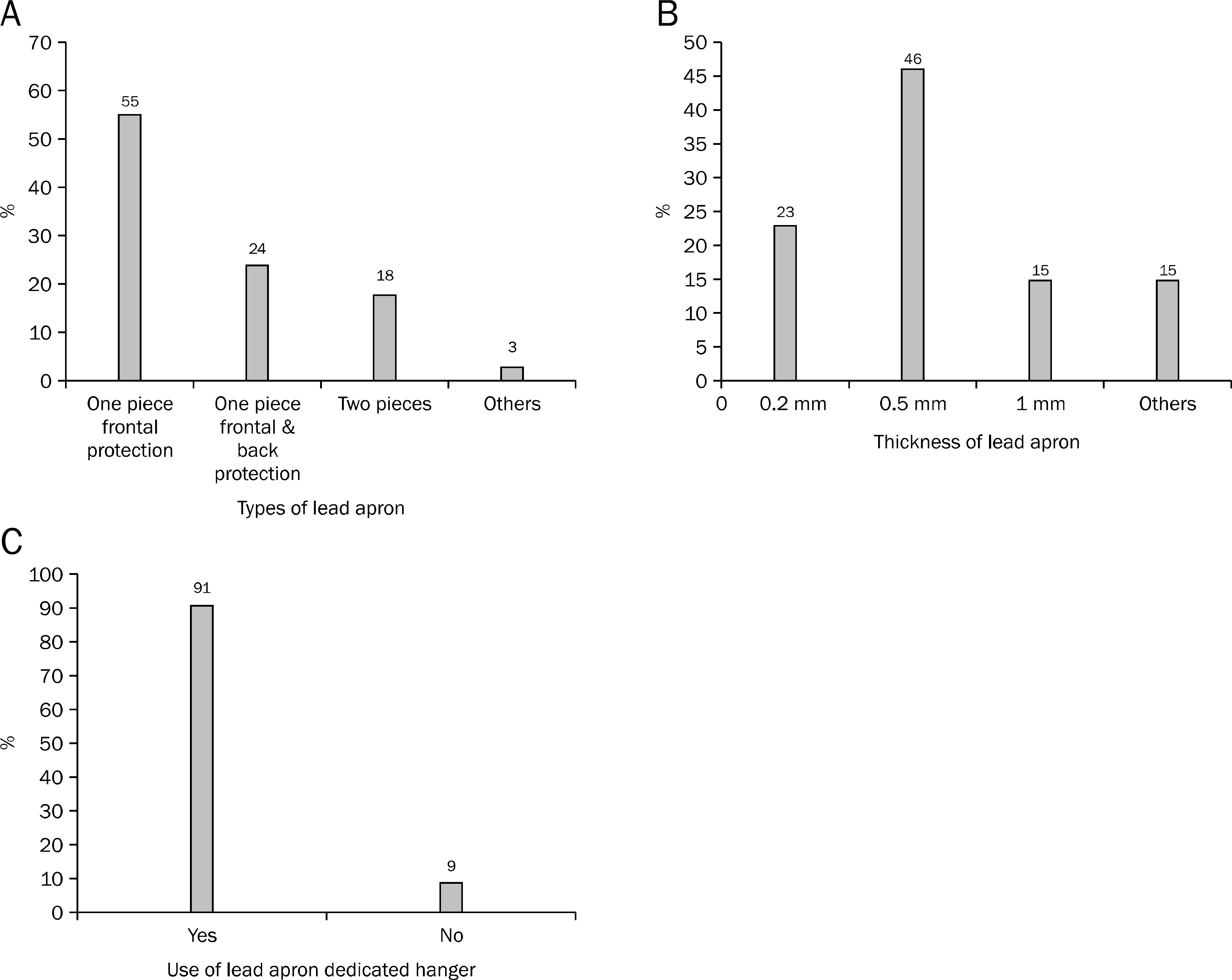
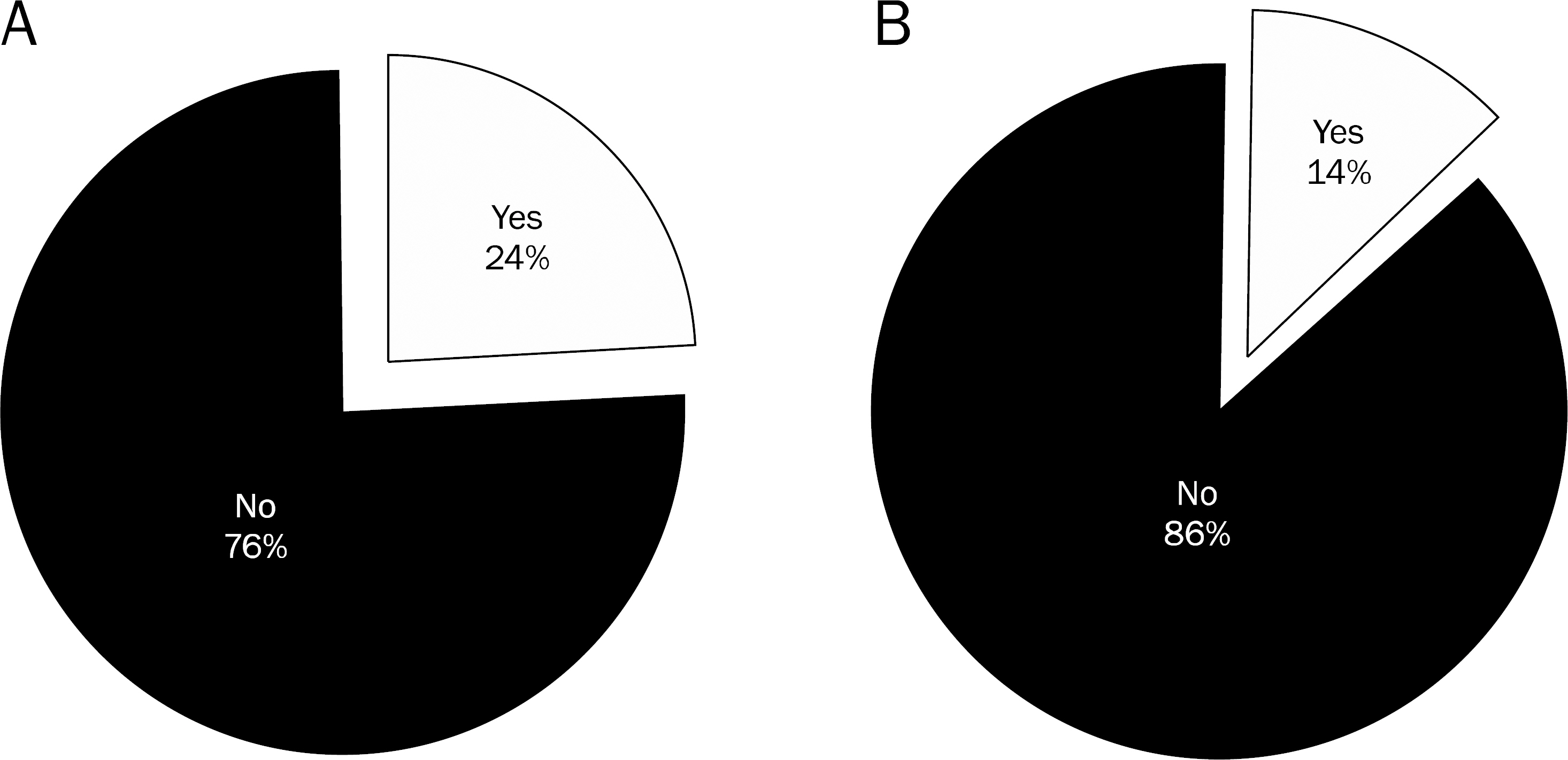
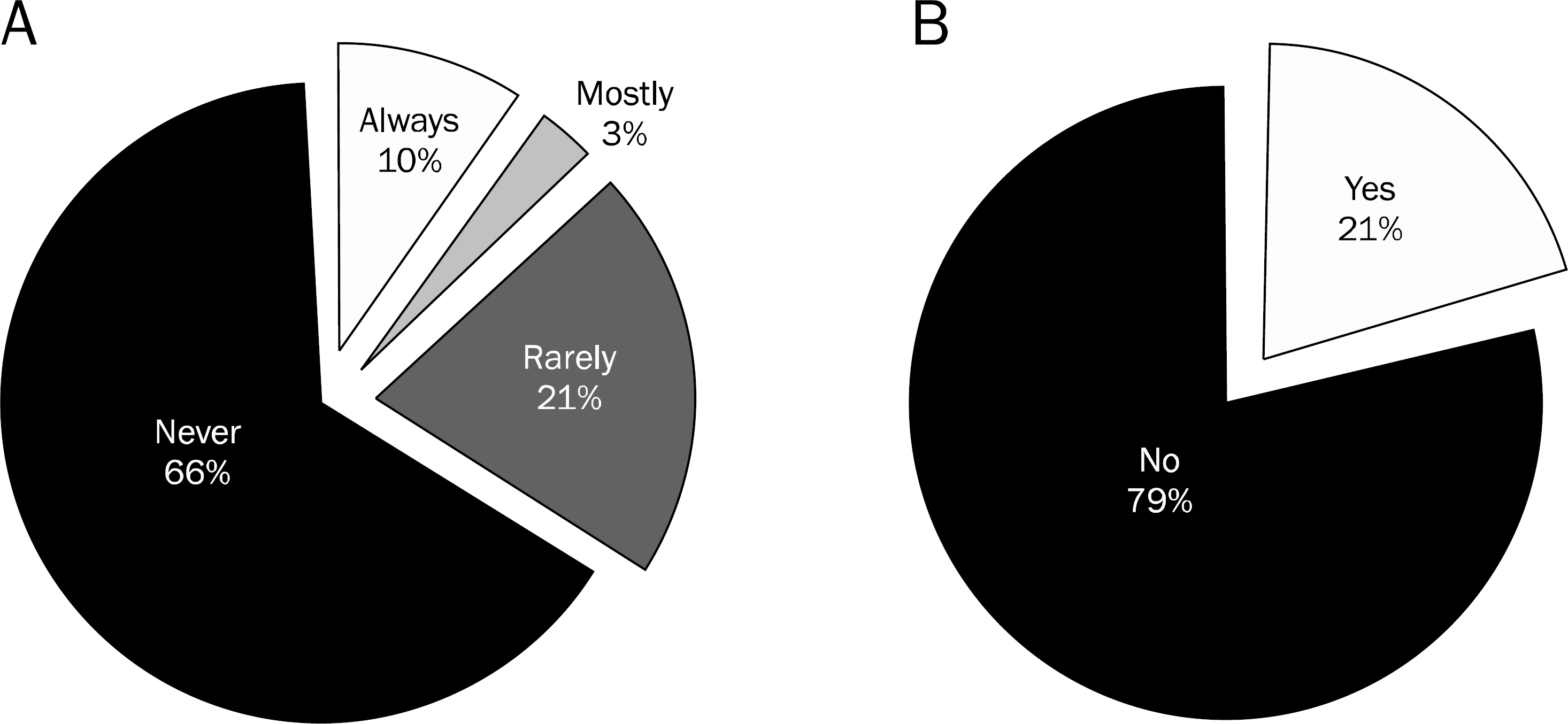
An anonymous questionnaire regarding radiation protection practices was mailed to 100 members of Korean Pancreatobiliary Association who was porforming ERCP. The questionnaire included ERCP volume of each endoscopist, use of protection devices such as apron, thyroid shield, lead glasses and any mobile shield for scattered radiation, and whether they monitored their own radiation exposure dosage.
RESULTS
All respondents wore lead aprons during ERCP. While 52.5% of endoscopists answered that they always wear thyroid guards, 26.9% rarely or never wore it. Only 14% wore lead glasses during the procedure and 69% never wore it. The preparation rates of mobile shields or lead curtains were only 14% and 24%, respectively. Only 10% of endoscopists attached an X-ray badge and 66.7% never used it. Moreover, 75% of endoscopists responded that they did not monitor their own exposure dose to radiation during ERCP.
CONCLUSIONS
The lack of radiation protection of ERCP endoscopists in Korea was seemed serious. Awareness of radiation hazard should be more concerned and educated in parallel with the preparation of radiation protection equipments.
MeSH Terms
Figure
Reference
-
References
1. Hendee WR. Estimation of radiation risks. BEIR V and its significance for medicine. JAMA. 1992; 268:620–624.
Article2. Kronenberg A. Radiation-induced genomic instability. Int J Radiat Biol. 1994; 66:603–609.
Article3. Russell WL. Comments on mutagenesis risk estimation. Genetics. 1979; 92(1 Suppl):S187–S194.4. Hall EJ. Scientific view of low-level radiation risks. Radiographics. 1991; 11:509–518.
Article5. Wrixon AD. New ICRP recommendations. J Radiol Prot. 2008; 28:161–168.
Article6. Bush WH, Jones D, Brannen GE. Radiation dose to personnel during percutaneous renal calculus removal. AJR Am J Roentgenol. 1985; 145:1261–1264.
Article7. McParland BJ, Nosil J, Burry B. A survey of the radiation exposures received by the staff at two cardiac catheterization laboratories. Br J Radiol. 1990; 63:885–888.
Article8. Ramsdale ML, Walker WJ, Horton PW. Extremity doses during interventional radiology. Clin Radiol. 1990; 41:34–36.
Article9. Campbell N, Sparrow K, Fortier M, Ponich T. Practical radiation safety and protection for the endoscopist during ERCP. Gastrointest Endosc. 2002; 55:552–557.
Article10. Naidu LS, Singhal S, Preece DE, Vohrah A, Loft DE. Radiation exposure to personnel performing endoscopic retrograde cholangiopancreatography. Postgrad Med J. 2005; 81:660–662.
Article11. Chen MY, Van Swearingen FL, Mitchell R, Ott DJ. Radiation exposure during ERCP: effect of a protective shield. Gastrointest Endosc. 1996; 43:1–5.
Article12. Cohen RV, Aldred MA, Paes WS, et al. How safe is ERCP to the endoscopist? Surg Endosc. 1997; 11:615–617.
Article13. Niklason LT, Marx MV, Chan HP. Interventional radiologists: oc-cupational radiation doses and risks. Radiology. 1993; 187:729–733.
Article14. Campbell N, Sparrow K, Fortier M, Ponich T. Practical radiation safety and protection for the endoscopist during ERCP. Gastrointest Endosc. 2002; 55:552–557.
Article15. Merriam GR Jr, Focht EF. A clinical study of radiation cataracts and the relationship to dose. Am J Roentgenol Radium Ther Nucl Med. 1957; 77:759–785.16. Kim YJ, Cho KB, Kim ES, et al. Efficacy of a self-designed protective lead shield in reduction of radiation exposure dose during endoscopic retrograde cholangiopancreatography. Korean J Gastroenterol. 2011; 57:28–33.
Article17. Geise RA, O'Dea TJ. Radiation dose in interventional fluoroscopic procedures. Appl Radiat Isot. 1999; 50:173–184.
Article18. Swayne LC, Lam SC, Filippone AL, Ambrose RB. Credentialing of crossover privileges in fluoroscopy for nonradiologists. Radiology. 1994; 190:281–282.
Article19. Thompson WL, Dyke JP, Buonocore E. Using the world-wide web to train and certify physicians in the safe use of fluoroscopy. AJR Am J Roentgenol. 1996; 166:1263–1264.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Retrograde Cholangiopancreatography in Post Gastrectomy Patients
- Minimizing radiation exposure in endoscopic retrograde cholangiopancreatography: a review for medical personnel
- Spyglass Direct Visualization System
- Efficacy of a Self-designed Protective Lead Shield in Reduction of Radiation Exposure Dose During Endoscopic Retrograde Cholangiopancreatography
- Practice of Endoscopic Retrograde Cholangiopancreatography in Korea: Results from a National Survey