Korean J Radiol.
2013 Dec;14(6):894-904. 10.3348/kjr.2013.14.6.894.
MR Imaging in Patients with Suspected Liver Metastases: Value of Liver-Specific Contrast Agent Gadoxetic Acid
- Affiliations
-
- 1Division of Abdominal Imaging, Department of Radiology, Seoul National University College of Medicine, Seoul 110-744, Korea. jmsh@snu.ac.kr
- 2Division of Abdominal Imaging, Department of Radiology, Seoul National University Bundang Hospital, Seongnam 463-767, Korea.
- 3Department of Radiology, Konkuk University School of Medicine, Seoul 143-701, Korea.
- KMID: 1711455
- DOI: http://doi.org/10.3348/kjr.2013.14.6.894
Abstract
OBJECTIVE
To compare the diagnostic performance of gadoxetic acid-enhanced magnetic resonance (MR) imaging with that of triple-phase multidetector-row computed tomography (MDCT) in the detection of liver metastasis.
MATERIALS AND METHODS
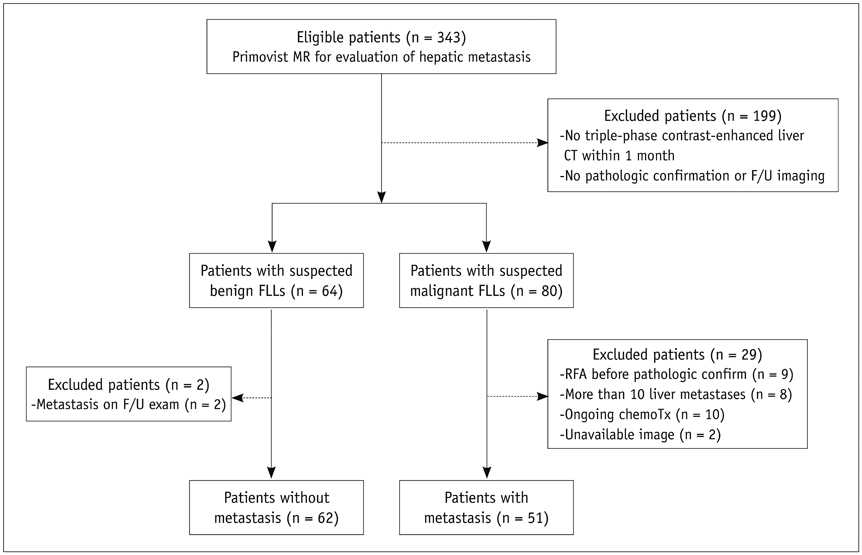
Our institutional review board approved this retrospective study and waived informed consent. The study population consisted of 51 patients with hepatic metastases and 62 patients with benign hepatic lesions, who underwent triple-phase MDCT and gadoxetic acid-enhanced MRI within one month. Two radiologists independently and randomly reviewed MDCT and MRI images regarding the presence and probability of liver metastasis. In order to determine additional value of hepatobiliary-phase (HBP), the dynamic-MRI set alone and combined dynamic-and-HBP set were evaluated, respectively. The standard of reference was a combination of pathology diagnosis and follow-up imaging. For each reader, diagnostic accuracy was compared using the jackknife alternative free-response receiver-operating-characteristic (JAFROC).
RESULTS
For both readers, average JAFROC figure-of-merit (FOM) was significantly higher on the MR image sets than on the MDCT images: average FOM was 0.582 on the MDCT, 0.788 on the dynamic-MRI set and 0.847 on the combined HBP set, respectively (p < 0.0001). The differences were more prominent for small (< or = 1 cm) lesions: average FOM values were 0.433 on MDCT, 0.711 on the dynamic-MRI set and 0.828 on the combined HBP set, respectively (p < 0.0001). Sensitivity increased significantly with the addition of HBP in gadoxetic acid-enhanced MR imaging (p < 0.0001).
CONCLUSION
Gadoxetic acid-enhanced MRI shows a better performance than triple-phase MDCT for the detection of hepatic metastasis, especially for small (< or = 1 cm) lesions.
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Contrast Media/diagnostic use
Diagnosis, Differential
Female
Gadolinium DTPA/*diagnostic use
Humans
Liver Neoplasms/*diagnosis/secondary
Magnetic Resonance Imaging/*methods
Male
Middle Aged
Multidetector Computed Tomography/methods
ROC Curve
Retrospective Studies
Contrast Media
Gadolinium DTPA
Figure
Reference
-
1. Zech CJ, Herrmann KA, Reiser MF, Schoenberg SO. MR imaging in patients with suspected liver metastases: value of liver-specific contrast agent Gd-EOB-DTPA. Magn Reson Med Sci. 2007; 6:43–52.2. Baker ME, Pelley R. Hepatic metastases: basic principles and implications for radiologists. Radiology. 1995; 197:329–337.3. Sica GT, Ji H, Ros PR. CT and MR imaging of hepatic metastases. AJR Am J Roentgenol. 2000; 174:691–698.4. Clemént O, Mühler A, Vexler VS, Kuwatsuru R, Berthezène Y, Rosenau W, et al. Comparison of Gd-EOB-DTPA and Gd-DTPA for contrast-enhanced MR imaging of liver tumors. J Magn Reson Imaging. 1993; 3:71–77.5. Halavaara J, Breuer J, Ayuso C, Balzer T, Bellin MF, Blomqvist L, et al. Liver tumor characterization: comparison between liver-specific gadoxetic acid disodium-enhanced MRI and biphasic CT--a multicenter trial. J Comput Assist Tomogr. 2006; 30:345–354.6. Huppertz A, Haraida S, Kraus A, Zech CJ, Scheidler J, Breuer J, et al. Enhancement of focal liver lesions at gadoxetic acid-enhanced MR imaging: correlation with histopathologic findings and spiral CT--initial observations. Radiology. 2005; 234:468–478.7. Vogl TJ, Kümmel S, Hammerstingl R, Schellenbeck M, Schumacher G, Balzer T, et al. Liver tumors: comparison of MR imaging with Gd-EOB-DTPA and Gd-DTPA. Radiology. 1996; 200:59–67.8. Muhi A, Ichikawa T, Motosugi U, Sou H, Nakajima H, Sano K, et al. Diagnosis of colorectal hepatic metastases: comparison of contrast-enhanced CT, contrast-enhanced US, superparamagnetic iron oxide-enhanced MRI, and gadoxetic acid-enhanced MRI. J Magn Reson Imaging. 2011; 34:326–335.9. Hamm B, Staks T, Mühler A, Bollow M, Taupitz M, Frenzel T, et al. Phase I clinical evaluation of Gd-EOB-DTPA as a hepatobiliary MR contrast agent: safety, pharmacokinetics, and MR imaging. Radiology. 1995; 195:785–792.10. Reimer P, Rummeny EJ, Shamsi K, Balzer T, Daldrup HE, Tombach B, et al. Phase II clinical evaluation of Gd-EOB-DTPA: dose, safety aspects, and pulse sequence. Radiology. 1996; 199:177–183.11. Kim SH, Kim SH, Lee J, Kim MJ, Jeon YH, Park Y, et al. Gadoxetic acid-enhanced MRI versus triple-phase MDCT for the preoperative detection of hepatocellular carcinoma. AJR Am J Roentgenol. 2009; 192:1675–1681.12. Kim YK, Lee YH, Kwak HS, Kim CS, Han YM. Detection of liver metastases: Gadoxetic acid-enhanced three-dimensional MR imaging versus ferucarbotran-enhanced MR imaging. Eur J Radiol. 2010; 73:131–136.13. Lee MH, Kim SH, Kim H, Lee MW, Lee WJ. Differentiating focal eosinophilic infiltration from metastasis in the liver with gadoxetic acid-enhanced magnetic resonance imaging. Korean J Radiol. 2011; 12:439–449.14. Park Y, Kim SH, Kim SH, Jeon YH, Lee J, Kim MJ, et al. Gadoxetic acid (Gd-EOB-DTPA)-enhanced MRI versus gadobenate dimeglumine (Gd-BOPTA)-enhanced MRI for preoperatively detecting hepatocellular carcinoma: an initial experience. Korean J Radiol. 2010; 11:433–440.15. Ward J. New MR techniques for the detection of liver metastases. Cancer Imaging. 2006; 6:33–42.16. Ichikawa T, Saito K, Yoshioka N, Tanimoto A, Gokan T, Takehara Y, et al. Detection and characterization of focal liver lesions: a Japanese phase III, multicenter comparison between gadoxetic acid disodium-enhanced magnetic resonance imaging and contrast-enhanced computed tomography predominantly in patients with hepatocellular carcinoma and chronic liver disease. Invest Radiol. 2010; 45:133–141.17. Doo KW, Lee CH, Choi JW, Lee J, Kim KA, Park CM. "Pseudo washout" sign in high-flow hepatic hemangioma on gadoxetic acid contrast-enhanced MRI mimicking hypervascular tumor. AJR Am J Roentgenol. 2009; 193:W490–W496.18. Löwenthal D, Zeile M, Lim WY, Wybranski C, Fischbach F, Wieners G, et al. Detection and characterisation of focal liver lesions in colorectal carcinoma patients: comparison of diffusion-weighted and Gd-EOB-DTPA enhanced MR imaging. Eur Radiol. 2011; 21:832–840.19. Shimada K, Isoda H, Hirokawa Y, Arizono S, Shibata T, Togashi K. Comparison of gadolinium-EOB-DTPA-enhanced and diffusion-weighted liver MRI for detection of small hepatic metastases. Eur Radiol. 2010; 20:2690–2698.20. Motosugi U, Ichikawa T, Onohara K, Sou H, Sano K, Muhi A, et al. Distinguishing hepatic metastasis from hemangioma using gadoxetic acid-enhanced magnetic resonance imaging. Invest Radiol. 2011; 46:359–365.21. Ahn SJ, Kim MJ, Hong HS, Kim KA, Song HT. Distinguishing hemangiomas from malignant solid hepatic lesions: a comparison of heavily T2-weighted images obtained before and after administration of gadoxetic acid. J Magn Reson Imaging. 2011; 34:310–317.22. Ba-Ssalamah A, Uffmann M, Saini S, Bastati N, Herold C, Schima W. Clinical value of MRI liver-specific contrast agents: a tailored examination for a confident non-invasive diagnosis of focal liver lesions. Eur Radiol. 2009; 19:342–357.23. Danet IM, Semelka RC, Leonardou P, Braga L, Vaidean G, Woosley JT, et al. Spectrum of MRI appearances of untreated metastases of the liver. AJR Am J Roentgenol. 2003; 181:809–817.24. Stern W, Schick F, Kopp AF, Reimer P, Shamsi K, Claussen CD, et al. Dynamic MR imaging of liver metastases with Gd-EOB-DTPA. Acta Radiol. 2000; 41:255–262.25. Motosugi U, Ichikawa T, Morisaka H, Sou H, Muhi A, Kimura K, et al. Detection of pancreatic carcinoma and liver metastases with gadoxetic acid-enhanced MR imaging: comparison with contrast-enhanced multi-detector row CT. Radiology. 2011; 260:446–453.26. Choi JW, Lee JM, Kim SJ, Yoon JH, Baek JH, Han JK, et al. Hepatocellular carcinoma: imaging patterns on gadoxetic acid-enhanced MR Images and their value as an imaging biomarker. Radiology. 2013; 267:776–786.27. Sun HY, Lee JM, Shin CI, Lee DH, Moon SK, Kim KW, et al. Gadoxetic acid-enhanced magnetic resonance imaging for differentiating small hepatocellular carcinomas (< or =2 cm in diameter) from arterial enhancing pseudolesions: special emphasis on hepatobiliary phase imaging. Invest Radiol. 2010; 45:96–103.28. Chakraborty DP. Analysis of location specific observer performance data: validated extensions of the jackknife free-response (JAFROC) method. Acad Radiol. 2006; 13:1187–1193.29. Chakraborty DP, Berbaum KS. Observer studies involving detection and localization: modeling, analysis, and validation. Med Phys. 2004; 31:2313–2330.30. Vikgren J, Zachrisson S, Svalkvist A, Johnsson AA, Boijsen M, Flinck A, et al. Comparison of chest tomosynthesis and chest radiography for detection of pulmonary nodules: human observer study of clinical cases. Radiology. 2008; 249:1034–1041.31. Zheng B, Chakraborty DP, Rockette HE, Maitz GS, Gur D. A comparison of two data analyses from two observer performance studies using Jackknife ROC and JAFROC. Med Phys. 2005; 32:1031–1034.32. Niekel MC, Bipat S, Stoker J. Diagnostic imaging of colorectal liver metastases with CT, MR imaging, FDG PET, and/or FDG PET/CT: a meta-analysis of prospective studies including patients who have not previously undergone treatment. Radiology. 2010; 257:674–684.33. Kulemann V, Schima W, Tamandl D, Kaczirek K, Gruenberger T, Wrba F, et al. Preoperative detection of colorectal liver metastases in fatty liver: MDCT or MRI? Eur J Radiol. 2011; 79:e1–e6.34. Park HS, Lee JM, Choi HK, Hong SH, Han JK, Choi BI. Preoperative evaluation of pancreatic cancer: comparison of gadolinium-enhanced dynamic MRI with MR cholangiopancreatography versus MDCT. J Magn Reson Imaging. 2009; 30:586–595.35. Lee JM, Zech CJ, Bolondi L, Jonas E, Kim MJ, Matsui O, et al. Consensus report of the 4th International Forum for Gadolinium-Ethoxybenzyl-Diethylenetriamine Pentaacetic Acid Magnetic Resonance Imaging. Korean J Radiol. 2011; 12:403–415.36. Kim YK, Ko SW, Hwang SB, Kim CS, Yu HC. Detection and characterization of liver metastases: 16-slice multidetector computed tomography versus superparamagnetic iron oxide-enhanced magnetic resonance imaging. Eur Radiol. 2006; 16:1337–1345.37. Motosugi U, Ichikawa T, Nakajima H, Sou H, Sano M, Sano K, et al. Imaging of small hepatic metastases of colorectal carcinoma: how to use superparamagnetic iron oxide-enhanced magnetic resonance imaging in the multidetector-row computed tomography age? J Comput Assist Tomogr. 2009; 33:266–272.38. Muhi A, Ichikawa T, Motosugi U, Sou H, Nakajima H, Sano K, et al. Diagnosis of colorectal hepatic metastases: Contrast-enhanced ultrasonography versus contrast-enhanced computed tomography versus superparamagnetic iron oxide-enhanced magnetic resonance imaging with diffusion-weighted imaging. J Magn Reson Imaging. 2010; 32:1132–1140.39. Onishi H, Murakami T, Kim T, Hori M, Iannaccone R, Kuwabara M, et al. Hepatic metastases: detection with multi-detector row CT, SPIO-enhanced MR imaging, and both techniques combined. Radiology. 2006; 239:131–138.40. Schwartz L, Brody L, Brown K, Covey A, Tuorto S, Mazumdar M, et al. Prospective, blinded comparison of helical CT and CT arterial portography in the assessment of hepatic metastasis from colorectal carcinoma. World J Surg. 2006; 30:1892–1899.41. Holzapfel K, Eiber MJ, Fingerle AA, Bruegel M, Rummeny EJ, Gaa J. Detection, classification, and characterization of focal liver lesions: Value of diffusion-weighted MR imaging, gadoxetic acid-enhanced MR imaging and the combination of both methods. Abdom Imaging. 2012; 37:74–82.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation and Prediction of Post-Hepatectomy Liver Failure Using Imaging Techniques: Value of Gadoxetic Acid-Enhanced Magnetic Resonance Imaging
- Supradiaphragmatic Liver Confirmed by a Hepatocyte-specific Contrast Agent (Gd-EOB-DTPA): A Case Report
- Current Limitations and Potential Breakthroughs for the Early Diagnosis of Hepatocellular Carcinoma
- Effect of Gadoxetic Acid on Quantification of Hepatic Steatosis Using Magnetic Resonance Spectroscopy: A Prospective Study
- Gadoxetic acid-enhanced magnetic resonance imaging: Hepatocellular carcinoma and mimickers