J Cardiovasc Ultrasound.
2013 Sep;21(3):103-112. 10.4250/jcu.2013.21.3.103.
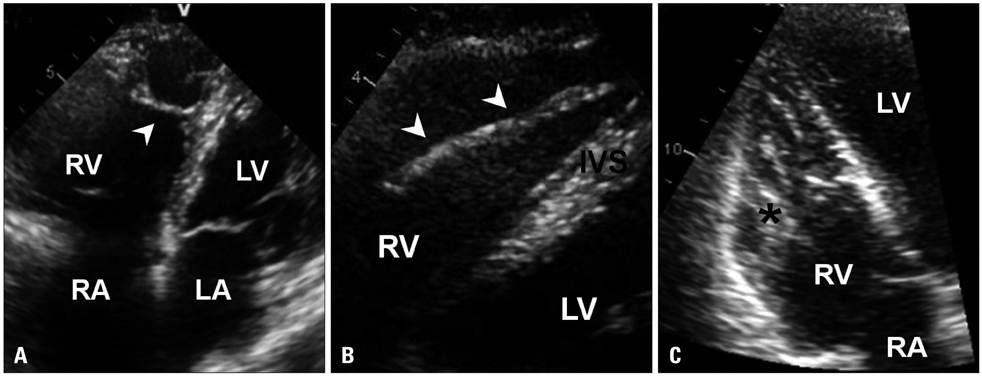
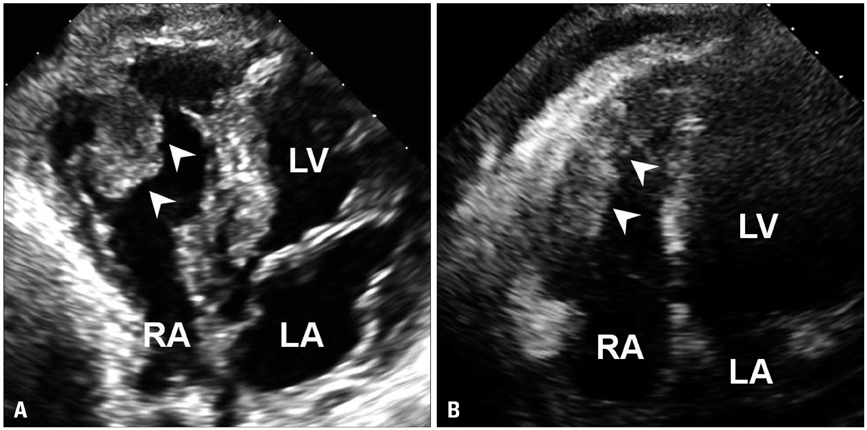
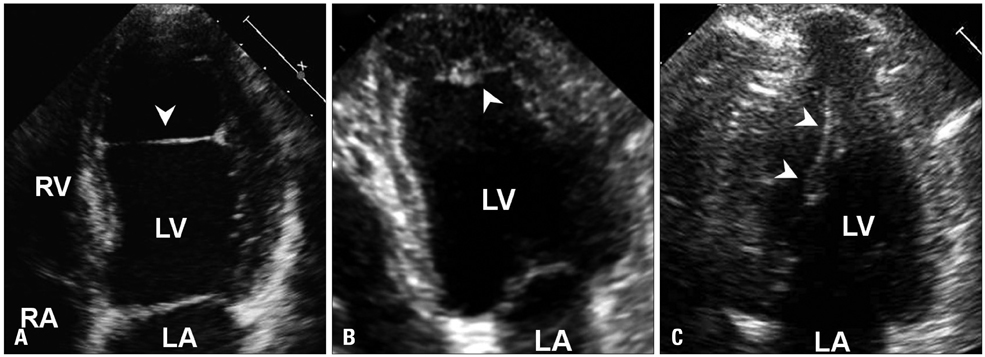
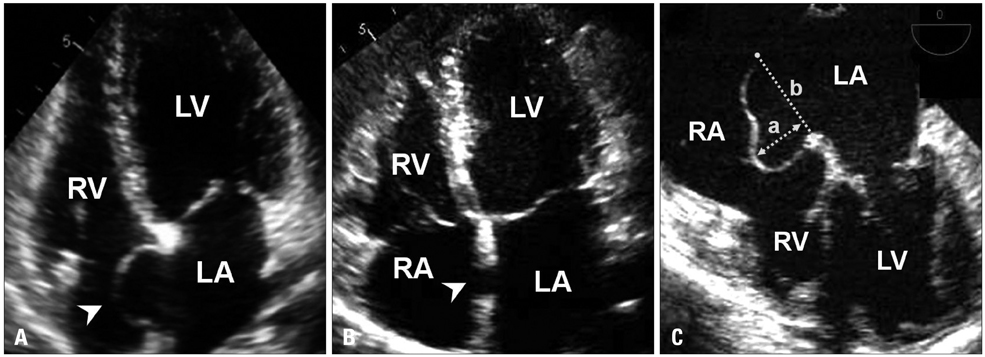
Anatomic Variants Mimicking Pathology on Echocardiography: Differential Diagnosis
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. hojheart@catholic.ac.kr
- KMID: 1500188
- DOI: http://doi.org/10.4250/jcu.2013.21.3.103
Abstract
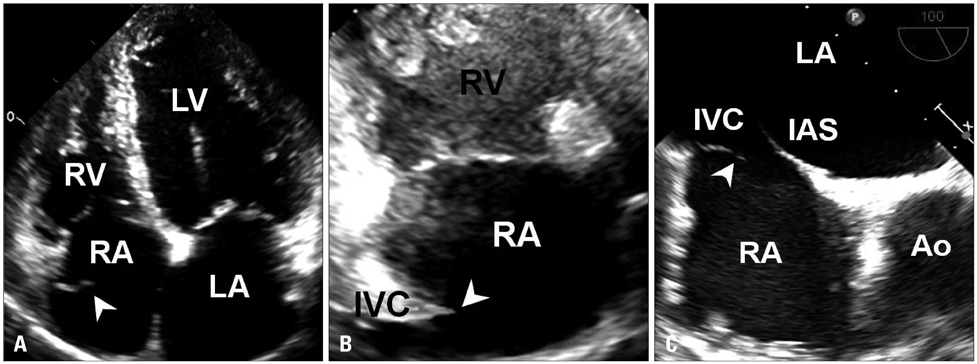
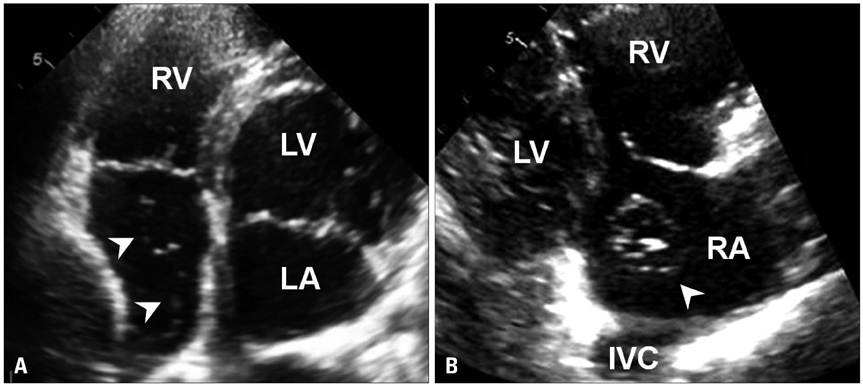
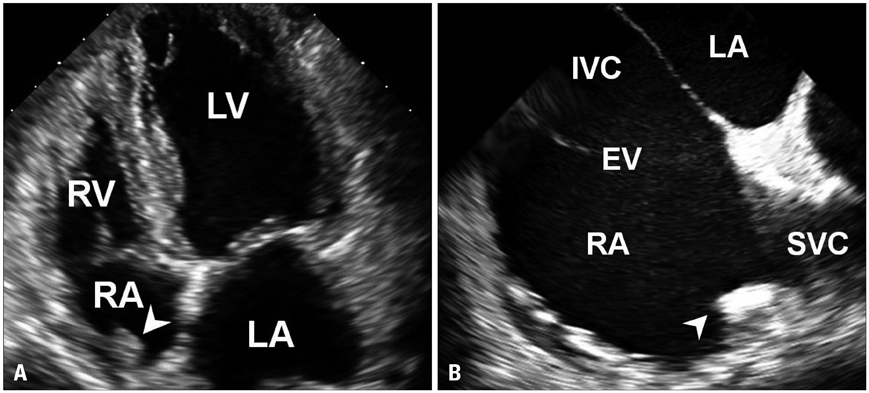
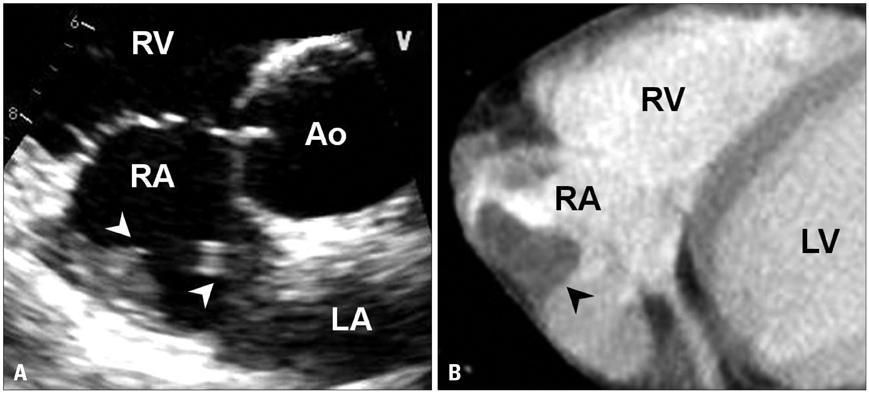
- Differentiation of normal from abnormal findings is critical in echocardiography. Anatomic variants occurring in normal cardiac developments often simulate pathologic entities. This review focuses on the differential diagnosis of normal anatomic structures from pathologic ones in echocardiography.
Keyword
Figure
Reference
-
1. Schoenwolf GC, Bleyl SB. Larsen's human embryology. 4th ed. Philadelphia: Churchill Livingstone/Elsevier;2009.2. Weyman AE. Principles and practice of echocardiography. 2nd ed. Philadelphia: Lippincott Williams & Wilkins;1994.3. Werner JA, Cheitlin MD, Gross BW, Speck SM, Ivey TD. Echocardiographic appearance of the Chiari network: differentiation from right-heart pathology. Circulation. 1981; 63:1104–1109.
Article4. Cooke JC, Gelman JS, Harper RW. Chiari network entanglement and herniation into the left atrium by an atrial septal defect occluder device. J Am Soc Echocardiogr. 1999; 12:601–603.
Article5. Goldschlager A, Goldschlager N, Brewster H, Kaplan J. Catheter entrapment in a Chiari network involving an atrial septal defect. Chest. 1972; 62:345–346.
Article6. Loukas M, Tubbs RS, Tongson JM, Polepalli S, Curry B, Jordan R, Wagner T. The clinical anatomy of the crista terminalis, pectinate muscles and the teniae sagittalis. Ann Anat. 2008; 190:81–87.
Article7. Mirowitz SA, Gutierrez FR. Fibromuscular elements of the right atrium: pseudomass at MR imaging. Radiology. 1992; 182:231–233.
Article8. Salustri A, Bakir S, Sana A, Lange P, Al Mahmeed WA. Prominent crista terminalis mimicking a right atrial mass: case report. Cardiovasc Ultrasound. 2010; 8:47.
Article9. Ports TA, Schiller NB, Strunk BL. Echocardiography of right ventricular tumors. Circulation. 1977; 56:439–447.
Article10. Nishimura T, Kondo M, Umadome H, Shimono Y. Echocardiographic features of the false tendons in the left ventricle. Am J Cardiol. 1981; 48:177–183.11. Keren A, Billingham ME, Popp RL. Echocardiographic recognition and implications of ventricular hypertrophic trabeculations and aberrant bands. Circulation. 1984; 70:836–842.
Article12. Luetmer PH, Edwards WD, Seward JB, Tajik AJ. Incidence and distribution of left ventricular false tendons: an autopsy study of 483 normal human hearts. J Am Coll Cardiol. 1986; 8:179–183.
Article13. George A, Parameswaran A, Nekkanti R, Lurito K, Movahed A. Normal anatomic variants on transthoracic echocardiogram. Echocardiography. 2009; 26:1109–1117.
Article14. Victor S, Nayak VM. Variations in the papillary muscles of the normal mitral valve and their surgical relevance. J Card Surg. 1995; 10:597–607.
Article15. Misra S, Koshy T, Pal S. Echo rounds: false tendons and accessory papillary muscle in the left ventricle. Anesth Analg. 2011; 113:1016–1018.16. Kwon DH, Setser RM, Thamilarasan M, Popovic ZV, Smedira NG, Schoenhagen P, Garcia MJ, Lever HM, Desai MY. Abnormal papillary muscle morphology is independently associated with increased left ventricular outflow tract obstruction in hypertrophic cardiomyopathy. Heart. 2008; 94:1295–1301.
Article17. Harrigan CJ, Appelbaum E, Maron BJ, Buros JL, Gibson CM, Lesser JR, Udelson JE, Manning WJ, Maron MS. Significance of papillary muscle abnormalities identified by cardiovascular magnetic resonance in hypertrophic cardiomyopathy. Am J Cardiol. 2008; 101:668–673.
Article18. Silver MD, Dorsey JS. Aneurysms of the septum primum in adults. Arch Pathol Lab Med. 1978; 102:62–65.19. Mügge A, Daniel WG, Angermann C, Spes C, Khandheria BK, Kronzon I, Freedberg RS, Keren A, Denning K, Engberding R, et al. Atrial septal aneurysm in adult patients. A multicenter study using transthoracic and transesophageal echocardiography. Circulation. 1995; 91:2785–2792.20. Hanley PC, Tajik AJ, Hynes JK, Edwards WD, Reeder GS, Hagler DJ, Seward JB. Diagnosis and classification of atrial septal aneurysm by two-dimensional echocardiography: report of 80 consecutive cases. J Am Coll Cardiol. 1985; 6:1370–1382.
Article21. Ong LS, Nanda NC, Falkoff MD, Barold SS. Interatrial septal aneurysm, systolic click and atrial tachyarrhythmia--a new syndrome? Ultrasound Med Biol. 1982; 8:691–693.
Article22. Mattioli AV, Aquilina M, Oldani A, Longhini C, Mattioli G. Atrial septal aneurysm as a cardioembolic source in adult patients with stroke and normal carotid arteries. A multicentre study. Eur Heart J. 2001; 22:261–268.
Article23. Page DL. Lipomatous hypertrophy of the cardiac interatrial septum: its development and probable clinical significance. Hum Pathol. 1970; 1:151–163.
Article24. Heyer CM, Kagel T, Lemburg SP, Bauer TT, Nicolas V. Lipomatous hypertrophy of the interatrial septum: a prospective study of incidence, imaging findings, and clinical symptoms. Chest. 2003; 124:2068–2073.25. Fyke FE 3rd, Tajik AJ, Edwards WD, Seward JB. Diagnosis of lipomatous hypertrophy of the atrial septum by two-dimensional echocardiography. J Am Coll Cardiol. 1983; 1:1352–1357.
Article26. Cunningham KS, Veinot JP, Feindel CM, Butany J. Fatty lesions of the atria and interatrial septum. Hum Pathol. 2006; 37:1245–1251.
Article27. Shirani J, Roberts WC. Clinical, electrocardiographic and morphologic features of massive fatty deposits ("lipomatous hypertrophy") in the atrial septum. J Am Coll Cardiol. 1993; 22:226–238.
Article28. Stephant E, Barthelet M, Leroux PY, Revel D. Images in cardiovascular medicine. Lipomatous hypertrophy of the interventricular septum: echocardiography, cardiac magnetic resonance, and multidetector computerized tomography imaging. Circulation. 2008; 118:e71–e72.29. Riva L, Banfi C, Gaeta R, Vigano M. Lipomatous hypertrophy of the interatrial septum. Description of a clinical case and literature review. Minerva Cardioangiol. 2006; 54:789–792.30. Armstrong WF, Ryan T. Feigenbaum's echocardiography. 7th ed. Philadelphia: Lippincott Williams & Wilkins;2010.31. Magarey FR. On the mode of formation of Lambl's excrescences and their relation to chronic thickening of the mitral valve. J Pathol Bacteriol. 1949; 61:203–208. 5 pl
Article32. Freedberg RS, Goodkin GM, Perez JL, Tunick PA, Kronzon I. Valve strands are strongly associated with systemic embolization: a transesophageal echocardiographic study. J Am Coll Cardiol. 1995; 26:1709–1712.
Article33. Roldan CA, Shively BK, Crawford MH. Valve excrescences: prevalence, evolution and risk for cardioembolism. J Am Coll Cardiol. 1997; 30:1308–1314.
Article34. Aziz F, Baciewicz FA Jr. Lambl's excrescences: review and recommendations. Tex Heart Inst J. 2007; 34:366–368.35. Klarich KW, Enriquez-Sarano M, Gura GM, Edwards WD, Tajik AJ, Seward JB. Papillary fibroelastoma: echocardiographic characteristics for diagnosis and pathologic correlation. J Am Coll Cardiol. 1997; 30:784–790.
Article36. Ngaage DL, Mullany CJ, Daly RC, Dearani JA, Edwards WD, Tazelaar HD, McGregor CG, Orszulak TA, Puga FJ, Schaff HV, Sundt TM 3rd, Zehr KJ. Surgical treatment of cardiac papillary fibroelastoma: a single center experience with eighty-eight patients. Ann Thorac Surg. 2005; 80:1712–1718.
Article37. Gowda RM, Khan IA, Nair CK, Mehta NJ, Vasavada BC, Sacchi TJ. Cardiac papillary fibroelastoma: a comprehensive analysis of 725 cases. Am Heart J. 2003; 146:404–410.
Article38. Lammers RJ, Bloor CM. Cancer and the heart. New York: Springer-Verlag;1986.39. Melduni RM, Klarich KW, Nesbitt GC, Shub C. Lambl's excrescences: is surgical excision really necessary? Tex Heart Inst J. 2008; 35:89. author reply 90.40. D'Avila A, Scanavacca M, Sosa E, Ruskin JN, Reddy VY. Pericardial anatomy for the interventional electrophysiologist. J Cardiovasc Electrophysiol. 2003; 14:422–430.