Korean J Radiol.
2013 Apr;14(2):154-163. 10.3348/kjr.2013.14.2.154.
Radiologists' Performance for Detecting Lesions and the Interobserver Variability of Automated Whole Breast Ultrasound
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea. lionmain@catholic.ac.kr
- 2Department of General Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- 3Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- 4CMC Clinical Research Coordinating Center, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- KMID: 1482772
- DOI: http://doi.org/10.3348/kjr.2013.14.2.154
Abstract
OBJECTIVE
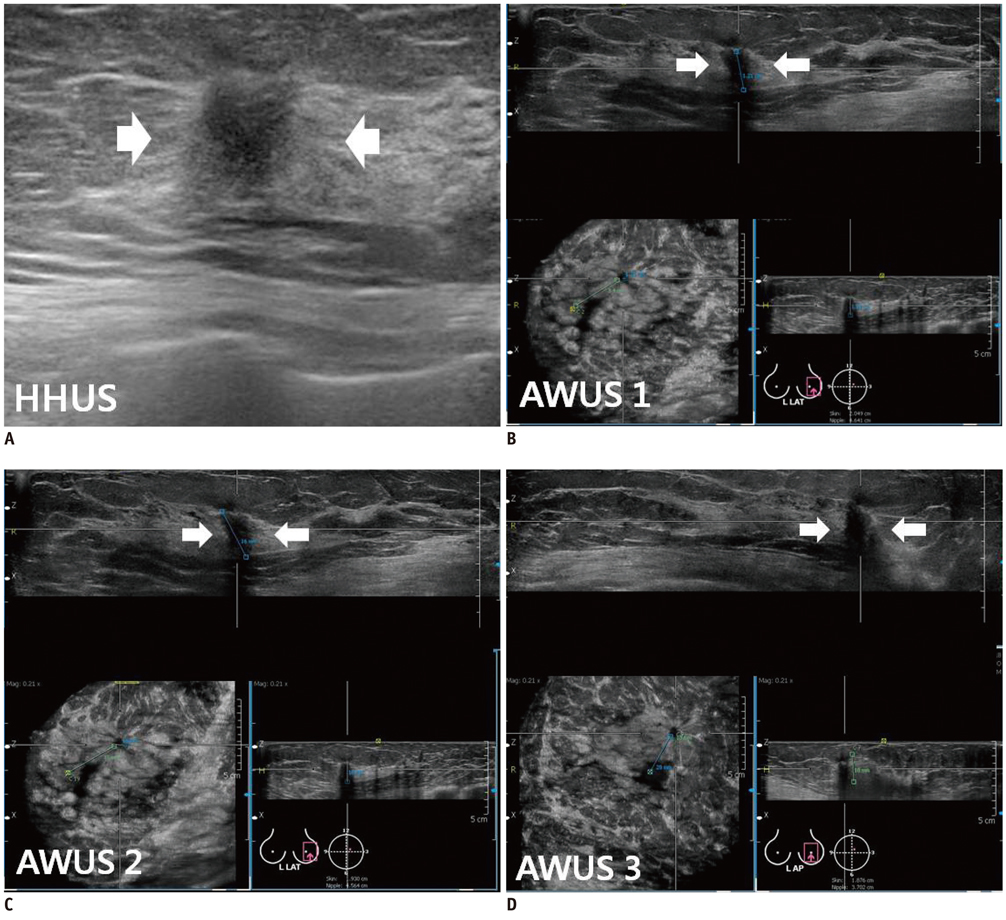
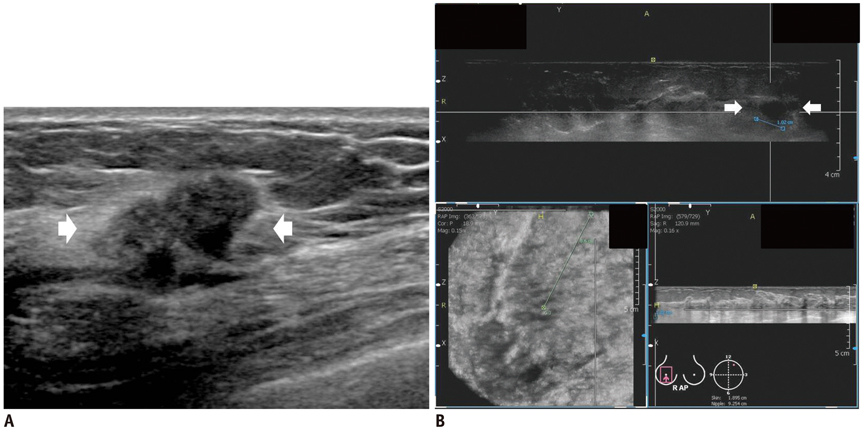
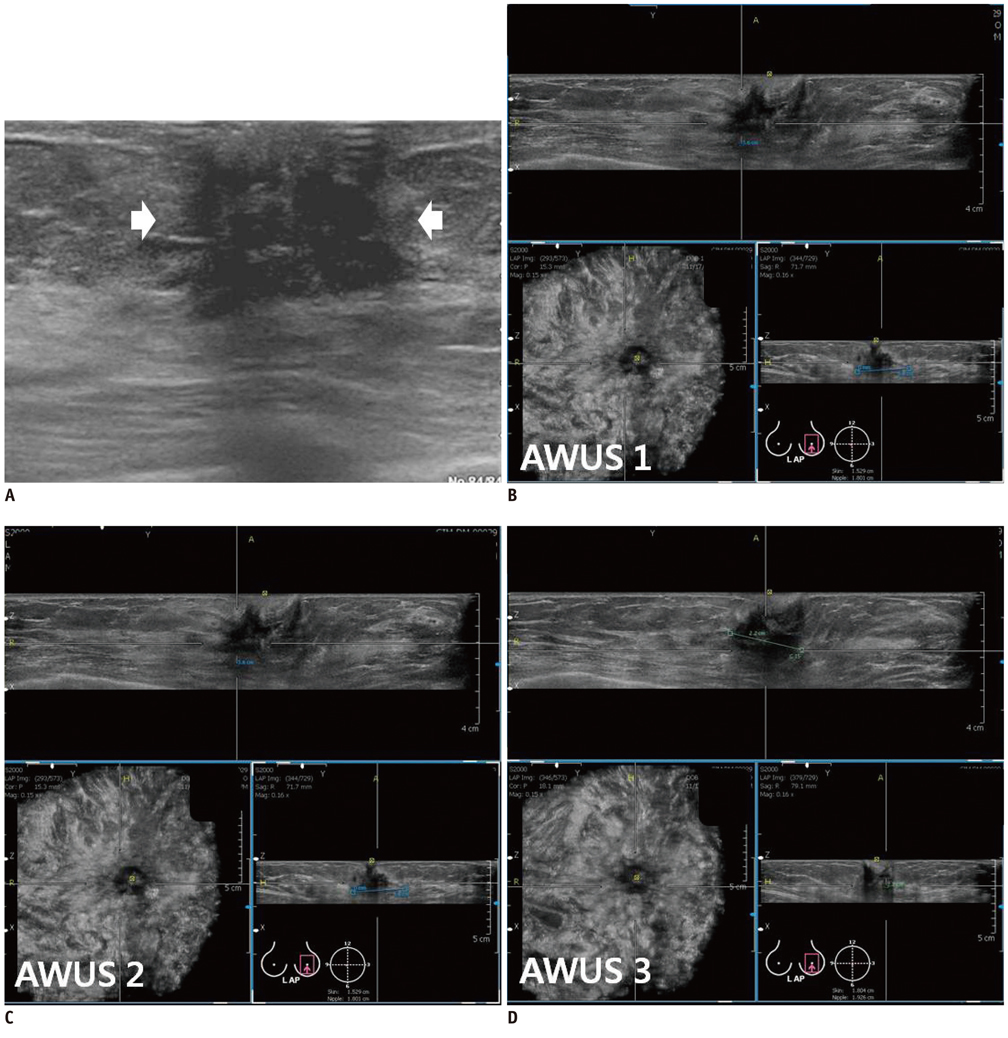
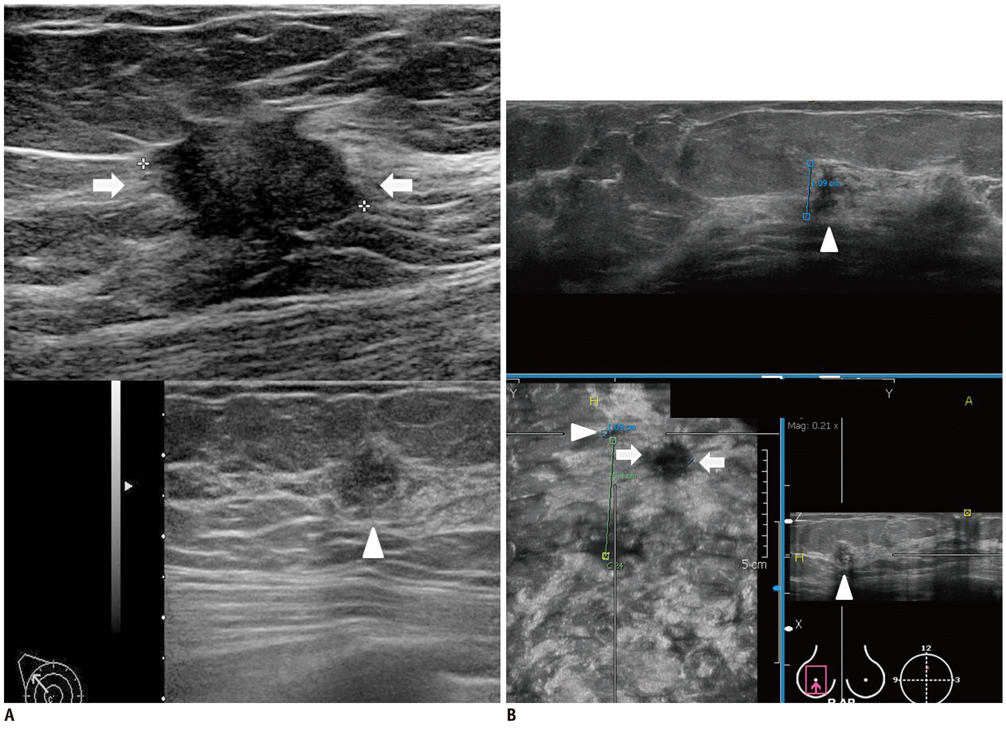
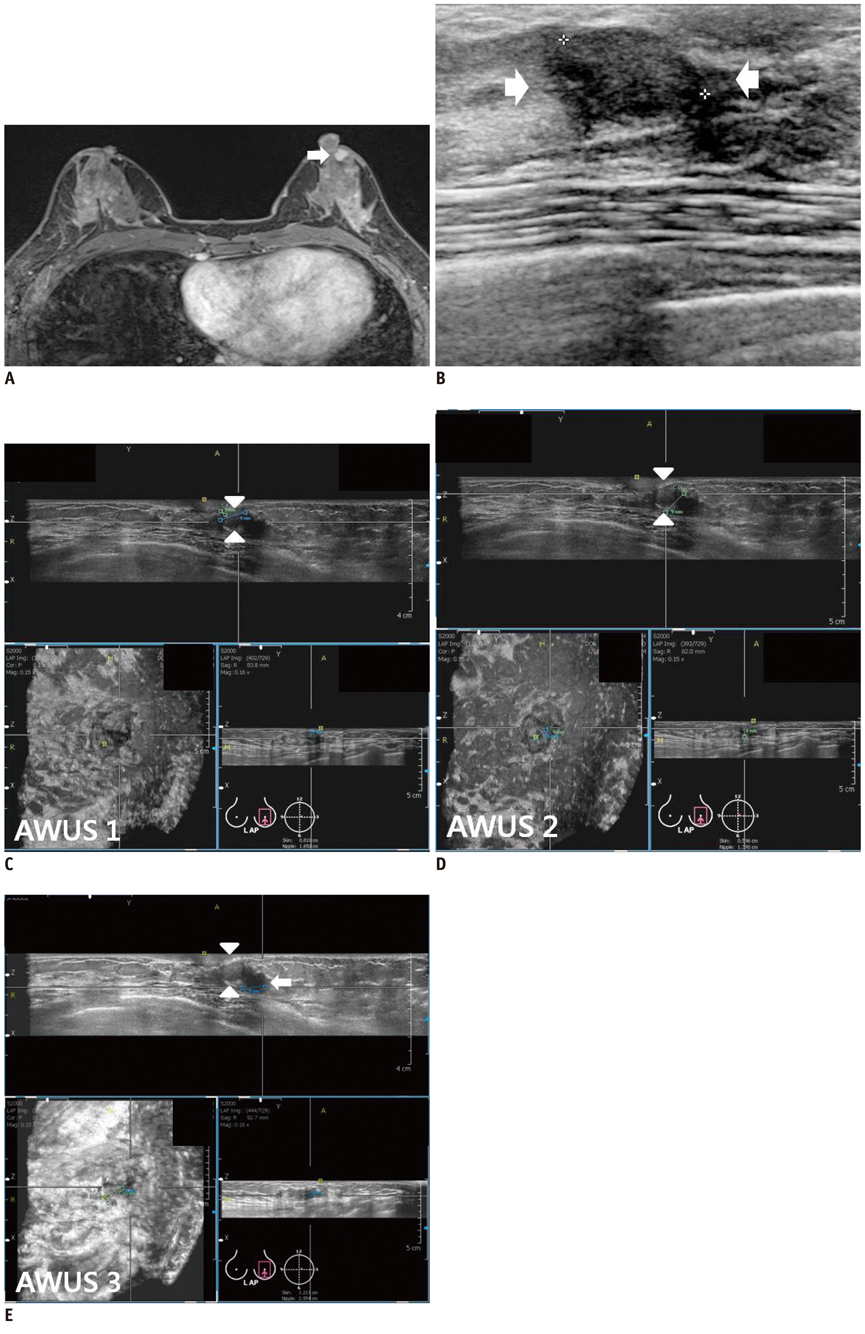
To compare the detection performance of the automated whole breast ultrasound (AWUS) with that of the hand-held breast ultrasound (HHUS) and to evaluate the interobserver variability in the interpretation of the AWUS.
MATERIALS AND METHODS
AWUS was performed in 38 breast cancer patients. A total of 66 lesions were included: 38 breast cancers, 12 additional malignancies and 16 benign lesions. Three breast radiologists independently reviewed the AWUS data and analyzed the breast lesions according to the BI-RADS classification.
RESULTS
The detection rate of malignancies was 98.0% for HHUS and 90.0%, 88.0% and 96.0% for the three readers of the AWUS. The sensitivity and the specificity were 98.0% and 62.5% in HHUS, 90.0% and 87.5% for reader 1, 88.0% and 81.3% for reader 2, and 96.0% and 93.8% for reader 3, in AWUS. There was no significant difference in the radiologists' detection performance, sensitivity and specificity (p > 0.05) between the two modalities. The interobserver agreement was fair to good for the ultrasonographic features, categorization, size, and the location of breast masses.
CONCLUSION
AWUS is thought to be useful for detecting breast lesions. In comparison with HHUS, AWUS shows no significant difference in the detection rate, sensitivity and the specificity, with high degrees of interobserver agreement.
Keyword
MeSH Terms
-
Aged
Breast Neoplasms/pathology/*ultrasonography
Chi-Square Distribution
*Clinical Competence
Diagnosis, Differential
Female
Humans
Image Interpretation, Computer-Assisted/methods
Magnetic Resonance Imaging
Middle Aged
Neoplasm Staging
Observer Variation
Sensitivity and Specificity
Ultrasonography, Mammary/*methods
Figure
Cited by 3 articles
-
Automated Breast Ultrasound Screening for Dense Breasts
Sung Hun Kim, Hak Hee Kim, Woo Kyung Moon
Korean J Radiol. 2020;21(1):15-24. doi: 10.3348/kjr.2019.0176.Detectability and Usefulness of Automated Whole Breast Ultrasound in Patients with Suspicious Microcalcifications on Mammography: Comparison with Handheld Breast Ultrasound
Jae Jeong Choi, Sung Hun Kim, Bong Joo Kang, Byung Joo Song
J Breast Cancer. 2016;19(4):429-437. doi: 10.4048/jbc.2016.19.4.429.Automated Breast Ultrasound: The Present and Future
Hyun Jo Youn, Ha Rim Ahn, Sang Yull Kang, Sung Hoo Jung
J Surg Ultrasound. 2022;9(2):23-29. doi: 10.46268/jsu.2022.9.2.23.
Reference
-
1. Chou YH, Tiu CM, Chen J, Chang RF. Automated full-field breast ultra-sonography: the past and the present. J Med Ultrasound. 2007. 15:31–44.2. Shipley JA, Duck FA, Goddard DA, Hillman MR, Halliwell M, Jones MG, et al. Automated quantitative volumetric breast ultrasound data-acquisition system. Ultrasound Med Biol. 2005. 31:905–917.3. Tozaki M, Fukuma E. Accuracy of determining preoperative cancer extent measured by automated breast ultrasonography. Jpn J Radiol. 2010. 28:771–773.4. Kotsianos-Hermle D, Wirth S, Fischer T, Hiltawsky KM, Reiser M. First clinical use of a standardized three-dimensional ultrasound for breast imaging. Eur J Radiol. 2009. 71:102–108.5. Chang JM, Moon WK, Cho N, Park JS, Kim SJ. Radiologists' performance in the detection of benign and malignant masses with 3D automated breast ultrasound (ABUS). Eur J Radiol. 2011. 78:99–103.6. Wenkel E, Heckmann M, Heinrich M, Schwab SA, Uder M, Schulz-Wendtland R, et al. Automated breast ultrasound: lesion detection and BI-RADS classification--a pilot study. Rofo. 2008. 180:804–808.7. Kotsianos-Hermle D, Hiltawsky KM, Wirth S, Fischer T, Friese K, Reiser M. Analysis of 107 breast lesions with automated 3D ultrasound and comparison with mammography and manual ultrasound. Eur J Radiol. 2009. 71:109–115.8. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. 33:159–174.9. Kelly KM, Dean J, Comulada WS, Lee SJ. Breast cancer detection using automated whole breast ultrasound and mammography in radiographically dense breasts. Eur Radiol. 2010. 20:734–742.10. Berg WA, Blume JD, Cormack JB, Mendelson EB. Operator dependence of physician-performed whole-breast US: lesion detection and characterization. Radiology. 2006. 241:355–365.11. Buchberger W, Niehoff A, Obrist P, DeKoekkoek-Doll P, Dünser M. Clinically and mammographically occult breast lesions: detection and classification with high-resolution sonography. Semin Ultrasound CT MR. 2000. 21:325–336.12. Schnarkowski P, Schmidt D, Milz P, Kessler M, Reiser MF. [Comparison between current and high resolution ultrasound for diagnosis of breast lesions]. Ultraschall Med. 1996. 17:190–194.13. Lazarus E, Mainiero MB, Schepps B, Koelliker SL, Livingston LS. BI-RADS lexicon for US and mammography: interobserver variability and positive predictive value. Radiology. 2006. 239:385–391.14. Park CS, Lee JH, Yim HW, Kang BJ, Kim HS, Jung JI, et al. Observer agreement using the ACR Breast Imaging Reporting and Data System (BI-RADS)-ultrasound, First Edition (2003). Korean J Radiol. 2007. 8:397–402.15. Lee HJ, Kim EK, Kim MJ, Youk JH, Lee JY, Kang DR, et al. Observer variability of Breast Imaging Reporting and Data System (BI-RADS) for breast ultrasound. Eur J Radiol. 2008. 65:293–298.16. Abdullah N, Mesurolle B, El-Khoury M, Kao E. Breast imaging reporting and data system lexicon for US: interobserver agreement for assessment of breast masses. Radiology. 2009. 252:665–672.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Technical Note on a Novel Technique for the Evaluation of Breast Excision Specimen: Automated Breast Ultrasound System
- The Interobserver Variability and Diagnostic Performance of 3-Dimensional Breast Ultrasound
- Usefulness of Ultrasound-Guided Automated Core Biopsy of Nonpalpable Breast Lesions
- Elastography of the Breast: Imaging Techniques and Pitfalls in Interpretation
- Automated Breast Ultrasound