J Korean Fract Soc.
2009 Apr;22(2):71-78. 10.12671/jkfs.2009.22.2.71.
Crescent Fracture-dislocation of Sacroiliac Joint: Affecting Factors of Operative Results
- Affiliations
-
- 1Department of Orthopedic Surgery, School of Medicine, Kyungpook National University, Daegu, Korea. cwoh@knu.ac.kr
- 2Department of Orthopedic Surgery, Daegu Veterans Hospital, Daegu, Korea.
- 3Department of Orthopedic Surgery, Daegu Fatima Hospital, Daegu, Korea.
- KMID: 1470018
- DOI: http://doi.org/10.12671/jkfs.2009.22.2.71
Abstract
-
PURPOSE: To assess the affecting factors of results after the operation of Crescent fracture-dislocation in sacro-iliac joint.
MATERIALS AND METHODS
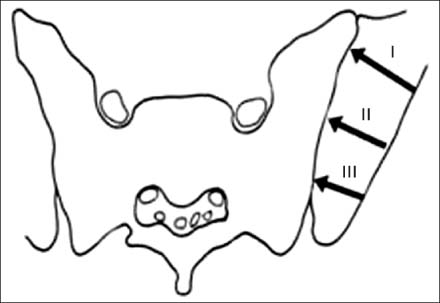
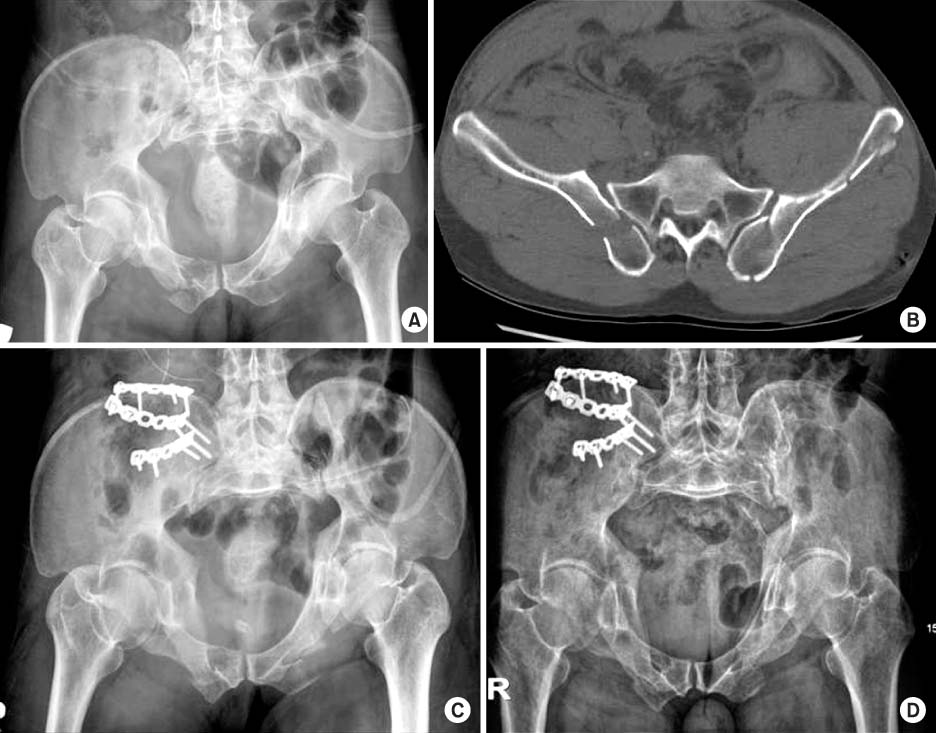
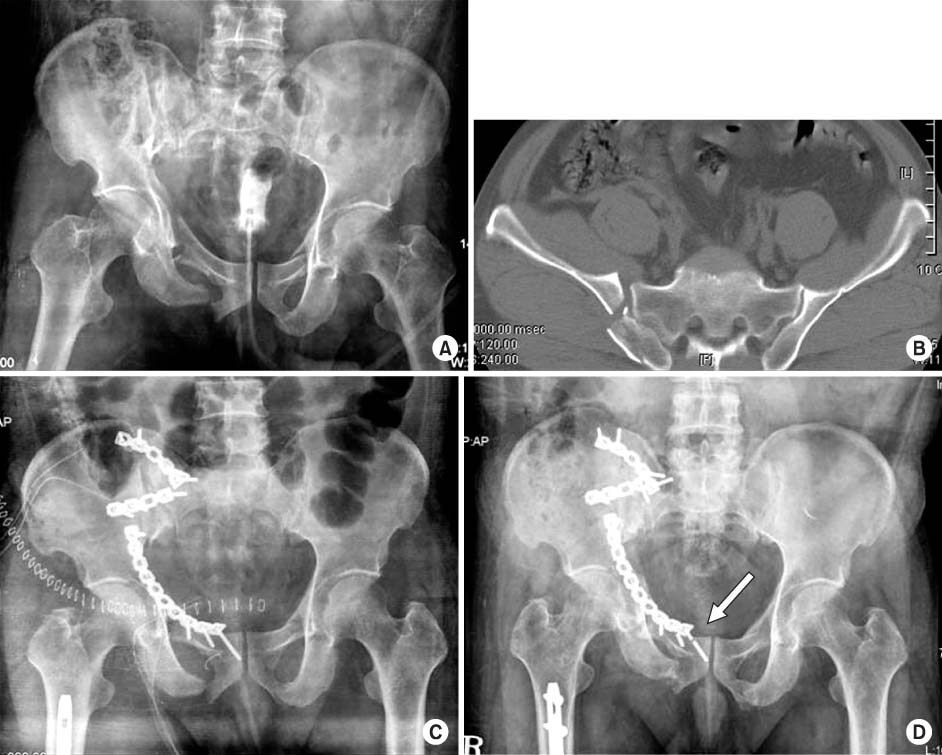
In 19 patients (mean age, 47.4 year-old) of open reduction and internal fixation for Crescent fracture-dislocation, there were seven type I, 9 type II, and 3 type III fractures according to Day's classification. We assessed affecting factors of radiological and functional results, such as patients' ages, surgical approaches, the fixation extent of pelvic ring, and fracture patterns.
RESULTS
Seventeen of 19 cases united at 14.5 weeks in average, and 2 non-unions occurred with the fixation failure of posterior ring. Satisfactory results were 14 and 15 in radiological and functional evaluation, respectively. In complications, three cases of leg length discrepancy were from an imperfect reduction and two fixation failures. Surgical approach did not show any difference of results, but all cases of unsatisfactory reduction occurred from posterior ring fixation through the anterior approach. Fixation of both rings seemed to have satisfactory results, comparing to posterior ring only. Older patients over 60 year-old had more complications and a tendency to show an unsatisfactory result.
CONCLUSION
In operative treatment of Crescent fracture-dislocation of sacro-iliac joint, it is better to fix both anterior and posterior rings. But, caution is needed to prevent complications in old-aged patients.
Figure
Cited by 2 articles
-
Damage Control and Provisional Fixation
Hyoung Keun Oh
J Korean Fract Soc. 2010;23(3):346-352. doi: 10.12671/jkfs.2010.23.3.346.General Assessment and Initial Management of Polytrauma Patients
Hyoung Keun Oh
J Korean Fract Soc. 2013;26(3):230-240. doi: 10.12671/jkfs.2013.26.3.230.
Reference
-
1. Bellabarba C, Ricci WM, Bolhofner BR. Distraction external fixation in lateral compression pelvic fractures. J Orthop Trauma. 2006; 20:1 Suppl. S7–S14.
Article2. Borrelli J Jr, Koval KJ, Helfet DL. The crescent fracture: a posterior fracture dislocation of the sacroiliac joint. J Orthop Trauma. 1996; 10:165–170.
Article3. Borrelli J Jr, Koval KJ, Helfet DL. Operative stabilization of fracture dislocations of the sacroiliac joint. Clin Orthop Relat Res. 1996; 329:141–146.
Article4. Burgess AR, Eastridge BJ, Young JW, et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990; 30:848–856.5. Day AC, Kinmont C, Bircher MD, Kumar S. Crescent fracture-dislocation of the sacroiliac joint: a functional classification. J Bone Joint Surg Br. 2007; 89:651–658.6. Ebraheim NA, Coombs R, Rusin JJ, Jackson WT, Holiday B. Percutaneous computed-tomography stabilization of pelvic fractures: preliminary report. J Orthop Trauma. 1987; 1:197–204.
Article7. Helfet DL. Open reduction internal fixation of the pelvis. Tech Orthop. 1990; 4:67–78.
Article8. Holdsworth FW. Dislocation and fracture-dislocation of the pelvis. J Bone Joint Surg Am. 1948; 30:461–466.
Article9. Kellam JF, McMurtry RY, Paley D, Tile M. The unstable pelvic fracture. Operative treatment. Orthop Clin North Am. 1987; 18:25–41.10. Kim PT, Oh CW, Ihn JC, Kwun JD. The biomechanical study on the extraction strengths of iliosacral lag screws. J Korean Soc Fract. 2000; 13:696–701.
Article11. Lee JY, Moon DH, Kim GB. Prognosis of early internal fixation in unstable pelvic fractures. J Korean Soc Fract. 2000; 13:741–748.
Article12. Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989; 242:83–97.
Article13. Pohlemann T, Bosch U, Gänsslen A, Tscherne H. The hannover experience in the management of pelvic fractures. Clin Orthop Relat Res. 1994; 305:69–80.14. Rommens PM, Hessmann MH. Staged reconstruction of pelvic ring disruption: differences in morbidity, mortality, radiologic results, and functional outcomes between B1, B2/B3, and C-type lesions. J Orthop Trauma. 2002; 16:92–98.
Article15. Routt ML Jr, Simonia PT, Mills WJ. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997; 11:584–589.
Article16. Shaw JA, Mino DE, Werner FW, Murray DG. Posterior stabilization of pelvic fractures by use of threaded compression rods. Case reports and mechanical testing. Clin Orthop Relat Res. 1985; 192:240–254.17. Simpson LA, Waddell JP, Leighton RK, Kellam JF, Tile M. Anterior approach and stabilization of the disrupted sacroiliac joint. J Trauma. 1987; 27:1332–1339.
Article18. Starr AJ, Walter JC, Harris RW, Reinert CM, Jones AL. Percutaneous screw fixation of fractures of the iliac wing and fracture-dislocations of the sacro-iliac joint (OTA Types 61-B2.2 and 61-B2.3, or Young-Burgess "lateral compression type II" pelvic fractures). J Orthop Trauma. 2002; 16:116–123.
Article19. Tile M. Pelvic fracture: operative versus non-operative treatment. Orthop Clin North Am. 1980; 11:423–464.20. Tseng S, Tornetta P 3rd. Percutaneous management of morel-lavallee lesions. J Bone Joint Surg Am. 2006; 88:92–105.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Atypical Pelvic Crescent Fracture Caused by Vertical Shear Force
- Intrapelvic Anterior Plate Fixation for Crescent Fracture-Dislocation of Sacroiliac Joint
- Dislocation of Fifth Carpornetacarpal Joint: Two Cases Report
- A Operative treatment of the three-part, four-part Fracture and Fracture dislocation in proximal humerus
- Treatment of Traumatic Sternoclavicular Joint Anterior Dislocation with a Sternal Fracture