Clin Exp Otorhinolaryngol.
2009 Mar;2(1):28-32. 10.3342/ceo.2009.2.1.28.
Clinical Presentation and Management of Jugular Foramen Paraganglioma
- Affiliations
-
- 1Department of Otorhinolaryngology, Yonsei University College of Medicine, Seoul, Korea. wsleemd@yumc.yonsei.ac.kr
- KMID: 1466560
- DOI: http://doi.org/10.3342/ceo.2009.2.1.28
Abstract
OBJECTIVES
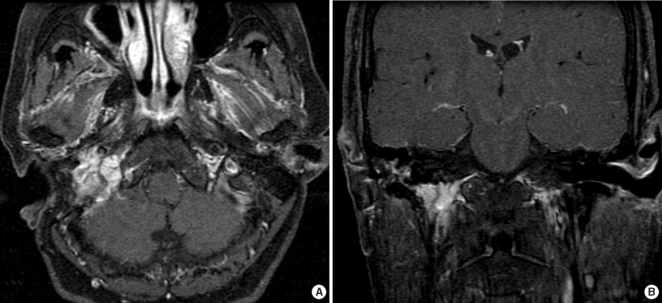
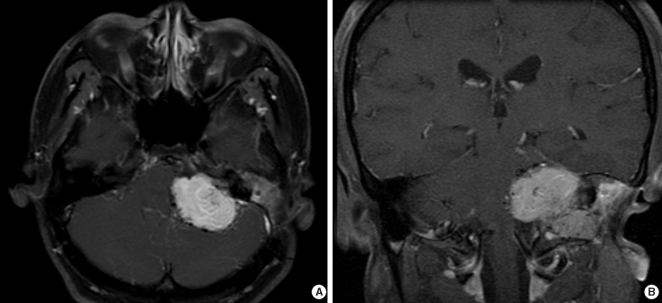
Jugular foramen paraganglioma is a locally invasive, benign tumor, which grow slowly and causes various symptoms such as pulsatile tinnitus and low cranial nerve palsy. Complete surgical resection is regarded as the ideal management of these tumors. The goal of this study is to identify the clinical characteristics and most effective surgical approach for jugular foramen paraganglioma.
METHODS
Retrospective analysis of 9 jugular foramen paraganglioma patients who underwent surgical resection between 1986 and 2005 was performed. Clinical records were reviewed for analysis of initial clinical symptoms and signs, audiological examinations, neurological deficits, radiological features, surgical approaches, extent of resection, treatment outcomes and complications.
RESULTS
Most common initial symptom was hoarseness, followed by pulsatile tinnitus. Seven out of 9 patients had at least one low cranial nerve palsy. Seven patients were classified as Fisch Type C tumor and remaining 2 as Fisch Type D tumor on radiologic examination. Total of 11 operations took place in 9 patients. Total resection was achieved in 6 cases, when partial resection was done in 3 cases. Two patients with partial resection received gamma knife radiosurgery (GKS), when remaining 1 case received both GKS and two times of revision operation. No mortality was encountered and there were few postoperative complications.
CONCLUSION
Neurologic examination of low cranial nerve palsy is crucial since most patients had at least one low cranial nerve palsy. All tumors were detected in advanced stage due to slow growing nature and lack of symptom. Angiography with embolization is crucial for successful tumor removal without massive bleeding. Infratemporal fossa approach can be considered as a safe, satisfactory approach for removal of jugular foramen paragangliomas. In tumors with intracranial extension, combined approach is recommended in that it provides better surgical view and can maintain the compliance of the patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Heth J. The basic science of glomus jugulare tumors. Neurosurg Focus. 2004; 8. 15. 17(2):E2. PMID: 15329017.
Article2. Ramina R, Maniglia JJ, Fernandes YB, Paschoal JR, Pfeilsticker LN, Neto MC, et al. Jugular foramen tumors: diagnosis and treatment. Neurosurg Focus. 2004; 8. 15. 17(2):E5. PMID: 15329020.
Article3. Al-Mefty O, Teixeira A. Complex tumors of the glomus jugulare: criteria, treatment, and outcome. J Neurosurg. 2002; 12. 97(6):1356–1366. PMID: 12507134.
Article4. Prabhu SS, DeMonte F. Complete resection of a complex glomus jugulare tumor with extensive venous involvement: case report. Neurosurg Focus. 2004; 8. 15. 17(2):E12. PMID: 15329027.5. Patel SJ, Sekhar LN, Cass SP, Hirsch BE. Combined approaches for resection of extensive glomus jugulare tumors. A review of 12 cases. J Neurosurg. 1994; 6. 80(6):1026–1038. PMID: 8189258.6. Coles MC. Glomus jugulare tumor presentation and management: a case study. J Neurosci Nurs. 2004; 8. 36(4):221–223. PMID: 15366548.
Article7. Watkins LD, Mendoza N, Cheesman AD, Symon L. Glomus jugulare tumours: a review of 61 cases. Acta Neurochir (Wien). 1994; 130(1-4):66–70. PMID: 7725944.
Article8. Michael LM 2nd, Robertson JH. Glomus jugulare tumors: historical overview of the management of this disease. Neurosurg Focus. 2004; 8. 15. 17(2):E1. PMID: 15329016.
Article9. Woods CI, Strasnick B, Jackson CG. Surgery for glomus tumors: the Otology Group experience. Laryngoscope. 1993; 11. 103(11 pt 2 suppl 60):65–70. PMID: 8231595.10. Mascarenhas F, Ferreira AG, Carvalho H, Almeida A, Santos M, Cattoni MB, et al. Kondziolka D, McDermott M, Régis J, Smee R, Flickinger JC, editors. Stereostatic radiosurgery in the management of glomus jugulare tumors. Radiosurgery. 2006. Basel: Karger;p. 108–117.11. Valavanis A. Preoperative embolization of the head and neck: indications, patient selection, goals, and precautions. AJNR Am J Neuroradiol. 1986; Sep–Oct. 7(5):943–952. PMID: 3096120.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of En Plaque Meningioma of Jugular Foramen with Image Findings of Differential Diagnosis
- Jugular foramen neurilemmoma mimicking an intra-axial brainstem tumor: a case report
- Paraganglioma of the Submandibular Region
- Jugular foramen paragangliomas: preoperative transcatheter particle embolization
- A Fatal Complication Associated with Combined Posterior Petrous and Suboccipital Approach to a Giant Jugular Foramen Schwannoma