J Korean Hip Soc.
2011 Dec;23(4):248-257. 10.5371/jkhs.2011.23.4.248.
Diagnosis and Treatment of Osteolysis
- Affiliations
-
- 1Department of Orthopedic Surgery, Soonchunhyang University Hospital, Seoul, Korea. yssuh@schmc.ac.kr
- KMID: 1452631
- DOI: http://doi.org/10.5371/jkhs.2011.23.4.248
Abstract
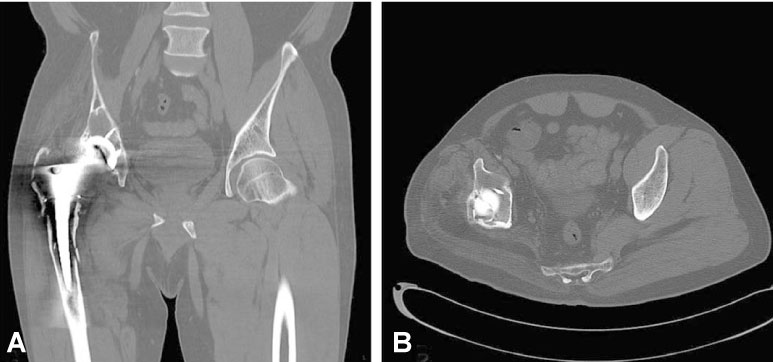
- Total hip replacement arthroplasty (THRA) is widely performed, and is a successful orthopedic treatment method. Osteolysis, which often happens after THRA, causes a chronic inflammation stage due to wear debris in the artificial articular surface, leading to bone loss or loosening of implants. Osteolysis eventually results in shortening the lifespan of the joint. Afterwards, many researchers reported on the basis of experiments with tissue cultivation that due to the influence of wear particles, the surrounding tissues of the implants as obtained during replacement and the surrounding cells of the implants are secreting enzymes, prostaglandin, cytokine, and the like that stimulate the formation of fibrous tissues or bone resorption by osteoclasts. At this time, THRA was a main cement fixation method, so researchers thought that the loose particles of cement were the cause of osteolysis and aseptic loosening, and so they named these symptoms "cement disease". However, despite the advancement of cement techniques and the use of cement-free implants, the osteolysis problem continued to rise, leading to polyethylene wear particles being regarded as the main cause of osteolysis, and naming these symptoms "particle disease". In this way attention was drawn to new wear particles, now that it is revealed that ultra-high-molecular-weight-polyethylene (UHMWPE) or metal particles constitute the main cause. However, because no symptoms arise until serious bone defects or loosening occurs, it is difficult to diagnose or treat the disease early on. Thus, based on updated hypotheses and theories, this study examines the pathophysiology of osteolysis following THRA, as well as the diagnosis and treatment of osteolysis in the acetabular and femoral regions.
Keyword
MeSH Terms
Figure
Reference
-
1. Willert HG, Semlitsch M. Reactions of the articular capsule to wear products of artificial joint protheses. J Biomed Mater Res. 1977. 11:157–164.
Article2. Willert HG, Ludwig J, Semlitsch M. Reaction of bone to methacrylate after hip arthroplasty: a long-term gross, light microscopic, and scanning electron microscopic study. J Bone Joint Surg Am. 1974. 56:1368–1382.3. Mirra JM, Amstutz HC, Matos M, Gold R. The pathology of the joint tissues and its clinical relevance in prosthesis failure. Clin Orthop Relat Res. 1976. 117:221–240.
Article4. Mirra JM, Marder RA, Amstutz HC. The pathology of the failed total joint arthroplasty. Clin Orthop Relat Res. 1982. 170:175–183.5. Goldring SR, Jasty M, Roelke MS, Rourke CM, Bringhurst FR, Harris WH. Formation of a synovial-like membrane at the bone-cement interface. Its role in bone resorption and implant loosening after total hip replacement. Arthritis Rheum. 1986. 29:836–842.
Article6. Goldring SR, Schiller AL, Roelke M, Rouke CM, O'Neil DA, Harris WH. The synovial-like membrane at the bone-cement interface in loose total hip replacements and its proposed role in bone lysis. J Bone Joint Surg Am. 1983. 65:575–584.
Article7. Arora A, Song Y, Chun L, et al. The role of the TH1 and TH2 immune response in loosening and osteolysis of cemented total hip replacements. J Biomed Mater Res A. 2003. 64:693–697.8. Shanbhag AS, Bailey HO, Hwang DS, Cha CW, Eror NG, Rubash HE. Quantitative analysis of ultrahigh molecular weight polyethylene (UHMWPE) wear debris associated with total knee replacements. J Biomed Mater Res. 2000. 53:100–110.
Article9. Haynes DR, Rodgers SD, Hay S, Pearcy MJ, Howie DW. The differences in toxicity and release of bone-resorbing mediators induced by titanium and cobalt-chromium-alloy wear particles. J Bone Joint Surg Am. 1993. 75:825–834.
Article10. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors govering bone ingrowth, stress shielding and clinical results. J Bone Joint Surg Br. 1987. 69:45–55.11. Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990. 257:107–128.
Article12. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969. 51:737–755.
Article13. Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg Am. 1995. 77:432–439.
Article14. Aspenberg P. Wear and osteolysis in total joint replacements. Acta Orthop Scand. 1998. 69:435–436.
Article15. Kadoya Y, Revel PA, al-Saffer N, Kobayashi A, Scott G, Freeman MA. Bone formation and bone resorption in failed total joint arthroplasties: histomorphometric analysis with histochemical and immunohistochemical technique. J Orthop Res. 1996. 14:473–482.
Article16. Shanbhag AS, Jacobs JJ, Black J, Galante JO, Glant TT. Human monocyte response to particulate biomaterials generated in vivo and in vitro. J Orthop Res. 1995. 13:792–801.
Article17. Fuller K, Murphy C, Kirstein B, Fox SW, Chambers TJ. TNFalpha potently activates osteoclasts, through a direct action independent of and strongly synergistic with RANKLE. Endocrinology. 2002. 143:1108–1118.
Article18. Lee SE, Chung WJ, Kwak HB, et al. Tumor necrosis factor-alpha supports the survival of osteoclasts through the activation of Akt and ERK. J Biol Chem. 2001. 276:49343–49349.
Article19. Stulberg SD, Wixson RL, Adams AD, Hendrix RW, Berfield JB. Monitoring pelvic osteolysis following total hip replacement surgery: an algorithm for surveillance. J Bone Joint Surg Am. 2002. 84-A:Suppl 2. 116–122.20. D'Antonio J, McCarthy JC, Bargar WL, et al. Classification of femoral abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1993. 296:133–139.21. Crawford RW, Evans M, Ling RS, Murray DW. Fluid flow around model femoral components of differing surface finishes: in vitro investigations. Acta Orthop Scand. 1999. 70:589–595.
Article22. Crawford RW, Psychoyios V, Gie G, Ling R, Murray D. Incomplete cement mantles in the sagittal femoral plane: an anatomical explanation. Acta Orthop Scand. 1999. 70:596–598.
Article23. Jacobs JJ, Roebuck KA, Archibeck M, Hallab NJ, Glant TT. Osteolysis:basic science. Clin Orthop Relat Res. 2001. 393:71–77.24. Gruen TA, McNeice GM, Amstutz HC. "Mode of failure" of cemented stem-type femoral componenets: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979. 141:17–27.25. Willert HG, Bertram H, Buchhorn GH. Osteolysis in alloarthroplasty of the hip. The role of bone cement fragmentation. Clin Orthop Relat Res. 1990. 258:108–121.26. Mulroy RD Jr, Harris WH. The effect of improved cementing techniques on component loosening in total hip replacement. An 11-year radiographic review. J Bone Joint Surg Br. 1990. 72:757–760.
Article27. Mulroy WF, Harris WH. Revision total hip arthroplasty with use of so-called second-generation cementing techniques for aseptic loosening of the femoral component. A fifteen-year-average follow-up study. J Bone Joint Surg Am. 1996. 78:325–330.
Article28. Maloney WJ, Woolson ST. Increasing incidence of femoral osteolysis in association with uncemented Harris-Galante total hip arthroplasty. A follow-up report. J Arthroplasty. 1996. 11:130–134.
Article29. Anthony PP, Gie GA, Howie CR, Ling RS. Localised endosteal bone lysis in relation to the femoral components of cemented total hip arthroplasties. J Bone Joint Surg Br. 1990. 72:971–979.
Article30. Emerson RH Jr, Sanders SB, Head WC, Higgins L. Effect of circumferential plasma-spray porous coating on the rate of femoral osteolysis after total hip arthroplasty. J Bone Joint Surg Am. 1999. 81:1291–1298.
Article31. Bobyn JD, Jacobs JJ, Tanzer M, et al. The susceptibility of smooth implant surfaces to periimplant fibrosis and migration of polyethylene wear debris. Clin Orthop Relat Res. 1995. 311:21–39.32. Wan Z, Dorr LD. Natural history of femoral focal osteolysis with proximal ingrowth smooth stem implant. J Arthroplasty. 1996. 11:718–725.
Article33. Engh CA, Hooten JP Jr, Zetti-Schaffer KF, et al. Porous-coated total hip replacement. Clin Orthop Relat Res. 1994. 298:89–96.
Article34. Hodgkinson JP, Shelley P, Wroblewski BM. The correlation between the roentgenographic appearance and operative findings at the bone-cement junction of the socket in Charley low friction arthroplasties. Clin Orthop Relat Res. 1988. 228:105–109.35. Stauffer RN. Ten-year follow-up study of total hip replacement. J Bone Joint Surg Am. 1982. 64:983–990.
Article36. Engh CA Jr, Sychterz CJ, Young AM, Pollock DC, Toomey SD, Engh CA Sr. Interovserver and intraobserver variability in radiographic assessment of osteolysis. J Arthroplasty. 2002. 17:752–759.
Article37. Moore KD, Barrack RL, Sychterz CJ, Sawhney J, Yang AM, Engh CA. The effect of weight bearing on the radiographic measurement of the position of the femoral head after total hip arthroplasty. J Bone Joint Surg Am. 2000. 82:62–69.
Article38. Pollock D, Sychterz CJ, Engh CA. A clinically practical method of manually assessing polyethylene liner thickness. J Bone Joint Surg Am. 2001. 83-A:1803.
Article39. Southwell DG, Bechtold JE, Lew WD, Schmidt AH. Improving the detection of acetabular osteolysis using oblique radiographs. J Bone Joint Surg Br. 1999. 81:289–295.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Diagnosis and Treatment of Femoral Osteolysis Developed after the Hip Replacement
- Osteolysis of the Distal Clavicle: Two Cases Report
- Osteolysis in Cementless Total Knee Arthroplasty
- Essential Osteolysis: A case report
- Band acro-osteolysis in a Black woman: a case report and review of the literature