J Korean Neurosurg Soc.
2012 Feb;51(2):86-90. 10.3340/jkns.2012.51.2.86.
Decompressive Hemicraniectomy and Duroplasty in Toddlers and Preschool Children with Refractory Intracranial Hypertension after Unilateral Hemispheric Stroke
- Affiliations
-
- 1Department of Neurosurgery, Korea University Ansan Hospital, Ansan, Korea. neuron19@korea.ac.kr
- KMID: 1441415
- DOI: http://doi.org/10.3340/jkns.2012.51.2.86
Abstract
OBJECTIVE
Life-threatening hemispheric stroke is associated with a high mortality and morbidity. Decompressive hemicraniectomy has been regarded as an effective treatment option for refractory intracranial hypertension. Here, we reported the clinical course of 5 children with decompressive craniectomy and duroplasty after non-traumatic refractory intracranial hypertension.
METHODS
Four toddlers and one preschool-girl were included in this study; there were 3 boys and 2 girls with a mean age of 34.6 months (range 17-80). Decompressive craniectomy including duroplasty was performed in cases of dilatation of pupil size after intensified standard medical therapy had proven insufficient. All children had a Pediatric Glasgow Coma Scale score <8 at pre-operation state. The mean time-point of craniectomy after stroke attack was 12 hours (range 4-19).
RESULTS
During the long-term follow-up period (mean 47.6 months), no children died. One year later, when we checked their Glasgow Outcome Scale scores, only one toddler received a score of 4 (moderate disability). But the others had good recoveries although they had minor physical or mental deficits. According to the Pediatric Cerebral Performance Category Scale, 4 children received a score of 2 (mild disability).
CONCLUSION
Despite our small cases, we suggest that decompressive hemicraniectomy and duroplasty is an acceptable and life-saving treatment for refractory intracranial hypertension after unilateral hemispheric stroke in toddlers and preschool children.
Keyword
MeSH Terms
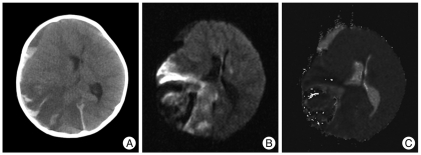
Figure
Reference
-
1. Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke : a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups : The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007; 115:e478–e534. PMID: 17515473.2. Aghakhani N, Durand P, Chevret L, Parker F, Devictor D, Tardieu M, et al. Decompressive craniectomy in children with nontraumatic refractory high intracranial pressure. Clinical article. J Neurosurg Pediatr. 2009; 3:66–69. PMID: 19119908.
Article3. Carter BS, Ogilvy CS, Candia GJ, Rosas HD, Buonanno F. One-year outcome after decompressive surgery for massive nondominant hemispheric infarction. Neurosurgery. 1997; 40:1168–1175. discussion 1175-1176. PMID: 9179889.
Article4. Chesnut RM. The management of severe traumatic brain injury. Emerg Med Clin North Am. 1997; 15:581–604. PMID: 9255134.
Article5. Chi CS, Law KL, Wong TT, Su GY, Lin N. Continuous monitoring of intracranial pressure in Reye's syndrome--5 years experience. Acta Paediatr Jpn. 1990; 32:426–434. PMID: 2288226.
Article6. Cho DY, Chen TC, Lee HC. Ultra-early decompressive craniectomy for malignant middle cerebral artery infarction. Surg Neurol. 2003; 60:227–232. discussion 232-233. PMID: 12922040.
Article7. Gordon AL, Ganesan V, Towell A, Kirkham FJ. Functional outcome following stroke in children. J Child Neurol. 2002; 17:429–434. PMID: 12174963.
Article8. Greenwood J Jr. Acute brain infarctions with high intracranial pressure : surgical indications. Johns Hopkins Med J. 1968; 122:254–260. PMID: 5655168.9. Gupta R, Connolly ES, Mayer S, Elkind MS. Hemicraniectomy for massive middle cerebral artery territory infarction : a systematic review. Stroke. 2004; 35:539–543. PMID: 14707232.
Article10. Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. 'Malignant' middle cerebral artery territory infarction : clinical course and prognostic signs. Arch Neurol. 1996; 53:309–315. PMID: 8929152.
Article11. Kirton A, deVeber G. Therapeutic approaches and advances in pediatric stroke. NeuroRx. 2006; 3:133–142. PMID: 16554252.
Article12. Lee MC, Frank JI, Kahana M, Tonsgard JH, Frim DM. Decompressive hemicraniectomy in a 6-year-old male after unilateral hemispheric stroke. Case report and review. Pediatr Neurosurg. 2003; 38:181–185. PMID: 12646736.
Article13. Lynch JK, Hirtz DG, DeVeber G, Nelson KB. Report of the National Institute of Neurological Disorders and Stroke workshop on perinatal and childhood stroke. Pediatrics. 2002; 109:116–123. PMID: 11773550.
Article14. Monagle P, Chan A, Massicotte P, Chalmers E, Michelson AD. Antithrombotic therapy in children : the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126:645S–687S. PMID: 15383489.15. Murphy S. Deaths : final data for 1998. Natl Vital Stat Rep. 2000; 48:1–105. PMID: 10934859.16. Ng LK, Nimmannitya J. Massive cerebral infarction with severe brain swelling : a clinicopathological study. Stroke. 1970; 1:158–163. PMID: 5522913.
Article17. Ramaswamy V, Mehta V, Bauman M, Richer L, Massicotte P, Yager JY. Decompressive hemicraniectomy in children with severe ischemic stroke and life-threatening cerebral edema. J Child Neurol. 2008; 23:889–894. PMID: 18403586.
Article18. Rieke K, Schwab S, Krieger D, von Kummer R, Aschoff A, Schuchardt V, et al. Decompressive surgery in space-occupying hemispheric infarction : results of an open, prospective trial. Crit Care Med. 1995; 23:1576–1587. PMID: 7664561.19. Tan MA, Salonga AM, Jamora RD. Decompressive hemicraniectomy in a 2-year-old girl with a left middle cerebral artery infarct. Childs Nerv Syst. 2006; 22:523–525. PMID: 16328393.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effectiveness of Decompressive Craniectomy with Dural Augmentation in Malignant Cerebral Infarction
- Effects of Decompressive Craniectomy for the Management of Patients with Refractory Intracranial Hypertension
- Where are We Now with Decompressive Hemicraniectomy for Malignant Middle Cerebral Artery Infarction?
- Therapeutic Hypothermia after Decompressive Craniectomy in Malignant Cerebral Infarction
- Surgical Management of Acute Infarction