J Korean Surg Soc.
2012 Dec;83(6):374-380. 10.4174/jkss.2012.83.6.374.
Clinical results between single incision laparoscopic cholecystectomy and conventional 3-port laparoscopic cholecystectomy: prospective case-matched analysis in single institution
- Affiliations
-
- 1Division of Hepatobiliary Surgery, Department of Surgery, Wonkwang University School of Medicine & Hospital, Iksan, Korea. chaekm@wonkwang.ac.kr
- KMID: 1437534
- DOI: http://doi.org/10.4174/jkss.2012.83.6.374
Abstract
- PURPOSE
The aim of our study was to compare single incision laparoscopic cholecystectomy (SILC) and conventional laparoscopic cholecystectomy (CLC) with respect to clinical outcomes.
METHODS
Patients with less than a 28 body mass index (BMI) and a benign gall bladder disease were enrolled in this study. From January 2011 to February 2012, 30 consecutive patients who underwent SILC were compared with 30 patients who underwent CLC during the same period. In this study, all operations were performed by one surgeon. In each group, patient characteristics and perioperative data were collected.
RESULTS
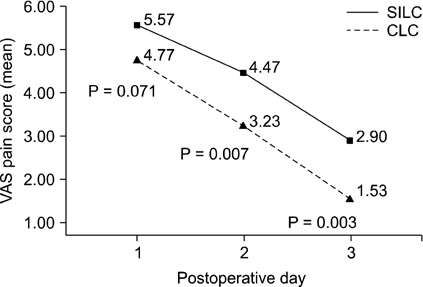
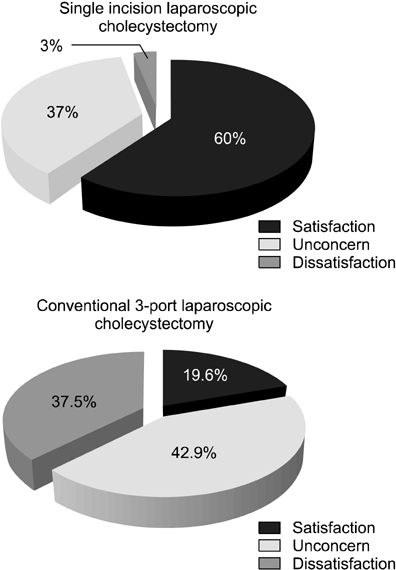
There was no significant difference in the preoperative characteristics. There was no significant difference in the postoperative laboratory result (alanine aminotransferase, aspartate aminotransferase, and alanine aminotransferase), number of conversion and complication cases, and length of hospital stay. The operation time was significantly longer in the SILC group (78.5 +/- 17.8 minutes in SILC group vs. 34.9 +/- 5.75 minutes in CLC group, P < 0.0001). The total nonsteroidal antiinflammatory drug usage during perioperative period showed significantly higher in SILC groups (162 +/- 51 mg in the SILC group vs. 138 +/- 30 mg in the CLC group), but there was no statistically significant difference in opioid usage between two groups. The postoperative pain score was significantly higher in the SILC group at second, third, and tenth postoperative day. Satisfaction of postoperative wound showed superiority in SILC group.
CONCLUSION
SILC seems to be an acceptable alternative to CLC with acceptable results. However, it is not enough to propose any real benefits of SILC when compared with CLC in terms of operation time and postoperative pain.
Keyword
MeSH Terms
Figure
Reference
-
1. Litynski GS. Erich Muhe and the rejection of laparoscopic cholecystectomy (1985): a surgeon ahead of his time. JSLS. 1998. 2:341–346.2. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997. 84:695.3. Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009. 23:1393–1397.4. Kim BS, Kim KC, Choi YB. A comparison between single-incision and conventional laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2012. 22:443–447.5. Choi SH, Hwang HK, Kang CM, Lee WJ. Single-fulcrum laparoscopic cholecystectomy: a single-incision and multi-port technique. ANZ J Surg. 2012. 82:529–534.6. Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P. Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc. 2012. 26:1205–1213.7. Han HJ, Choi SB, Kim WB, Choi SY. Single-incision multiport laparoscopic cholecystectomy: things to overcome. Arch Surg. 2011. 146:68–73.8. Lai EC, Yang GP, Tang CN, Yih PC, Chan OC, Li MK. Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Am J Surg. 2011. 202:254–258.9. Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. 2011. 98:1695–1702.10. Wang D, Wang Y, Ji ZL. Laparoendoscopic single-site cholecystectomy versus conventional laparoscopic cholecystectomy: a systematic review of randomized controlled trials. ANZ J Surg. 2012. 82:303–310.11. Roberts KE, Solomon D, Duffy AJ, Bell RL. Single-incision laparoscopic cholecystectomy: a surgeon's initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg. 2010. 14:506–510.12. Solomon D, Bell RL, Duffy AJ, Roberts KE. Single-port cholecystectomy: small scar, short learning curve. Surg Endosc. 2010. 24:2954–2957.13. Sasaki K, Watanabe G, Matsuda M, Hashimoto M. Original single-incision laparoscopic cholecystectomy for acute inflammation of the gallbladder. World J Gastroenterol. 2012. 18:944–951.14. Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc. 2010. 24:1403–1412.15. Feinberg EJ, Agaba E, Feinberg ML, Camacho D, Vemulapalli P. Single-incision laparoscopic cholecystectomy learning curve experience seen in a single institution. Surg Laparosc Endosc Percutan Tech. 2012. 22:114–117.16. Garg P, Thakur JD, Garg M, Menon GR. Single-incision laparoscopic cholecystectomy vs. conventional laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg. 2012. 16:1618–1628.17. Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S. Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg. 2011. 254:22–27.18. Garg P, Thakur JD, Raina NC, Mittal G, Garg M, Gupta V. Comparison of cosmetic outcome between single-incision laparoscopic cholecystectomy and conventional laparoscopic cholecystectomy: an objective study. J Laparoendosc Adv Surg Tech A. 2012. 22:127–130.19. Hey J, Roberts KJ, Morris-Stiff GJ, Toogood GJ. Patient views through the keyhole: new perspectives on single-incision vs. multiport laparoscopic cholecystectomy. HPB (Oxford). 2012. 14:242–246.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Single-Incision Robotic Cholecystectomy, Single-Incision Laparoscopic Cholecystectomy and 3-Port Laparoscopic Cholecystectomy -Postoperative Pain, Cosmetic Outcome and Surgeon's Workload
- Current Status of Single-port Colectomy in Korea
- Current Status of Single-port Laparoscopic Cholecystectomy
- Single Port Laparoscopic Cholecystectomy in a Patient with Situs Inversus Totalis: A Case Report
- Single-port Laparoscopic Cholecystectomy: Comparative Study of Consecutive Initial 206 Cases