J Korean Fract Soc.
2012 Oct;25(4):263-268. 10.12671/jkfs.2012.25.4.263.
Analysis of the Factors Involved in Failed Fixation in Elderly Intertrochanteric Femoral Fracture
- Affiliations
-
- 1Department of Orthopedic Surgery, Inha University School of Medicine, Incheon, Korea. kangjoon@inha.ac.kr
- KMID: 1434064
- DOI: http://doi.org/10.12671/jkfs.2012.25.4.263
Abstract
- PURPOSE
To analyze the causes of internal fixation failure in elderly intertrochanteric femoral fractures.
MATERIALS AND METHODS
We retrospectively analyzed 93 intertrochanteric femoral fractures that were treated by internal fixation. The follow-up period was at least 24 months. The mean age was 73 years. We analyzed the classification of the fracture, screw position, reduction state of the fracture, and neck-shaft angle.
RESULTS
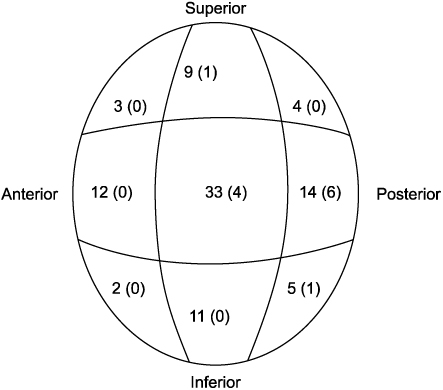
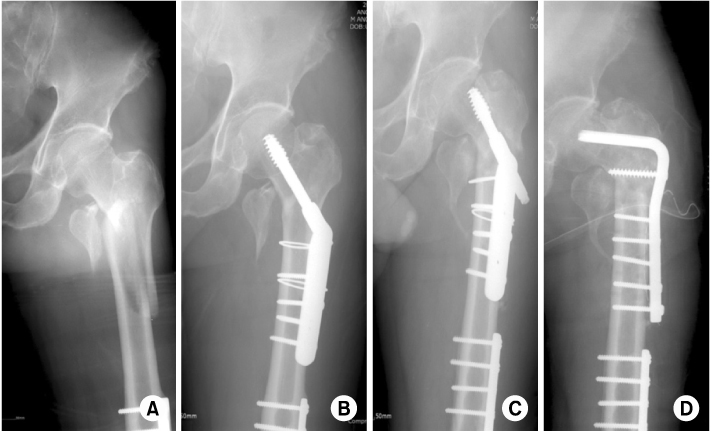
Internal fixation failure occurred in 12 cases (12.9%). The causes of internal fixation failure were one case (1.0%) of head perforation, 7 cases (7.5%) of excessive slippage of a screw, and 4 cases (4.3%) of varus deformity. Significant factors infixation failure were displacement of the posterolateral fragment more than 8 mm in anteroposterior radiograph, anterior displacement of a fragment, or more than 20-degree angulation in lateral radiography. Thirty-three cases had a screw in the middle position and 4 of these cases (12.1%) had fixation failure. Notably, 14 cases had a screw in the posteromedial position and 6 of these cases had fixation failure (42.8%).
CONCLUSION
Accurate reduction of the posteromedial fragment is essential in unstable intertrochanteric fracture and anterior displacement or angulation should be avoided to prevent fixation failure. The tip apex distance of the screw and central location of the screw in the femoral head is also an important factor.
Keyword
MeSH Terms
Figure
Reference
-
1. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995. 77:1058–1064.
Article2. Chirodian N, Arch B, Parker MJ. Sliding hip screw fixation of trochanteric hip fractures: outcome of 1024 procedures. Injury. 2005. 36:793–800.
Article3. Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br. 1990. 72:26–31.
Article4. Den Hartog BD, Bartal E, Cooke F. Treatment of the unstable intertrochanteric fracture. Effect of the placement of the screw, its angle of insertion, and osteotomy. J Bone Joint Surg Am. 1991. 73:726–733.
Article5. Doppelt SH. The sliding compression screw--today's best answer for stabilization of intertrochanteric hip fractures. Orthop Clin North Am. 1980. 11:507–523.
Article6. Flores LA, Harrington IJ, Heller M. The stability of intertrochanteric fractures treated with a sliding screw-plate. J Bone Joint Surg Br. 1990. 72:37–40.
Article7. Forte ML, Virnig BA, Kane RL, et al. Geographic variation in device use for intertrochanteric hip fractures. J Bone Joint Surg Am. 2008. 90:691–699.
Article8. Gargan MF, Gundle R, Simpson AH. How effective are osteotomies for unstable intertrochanteric fractures? J Bone Joint Surg Br. 1994. 76:789–792.
Article9. Guerra Pinto F, Dantas P, Moreira R, Mamede R, Amaral LB. Complications relating to accuracy of reduction of intertrochanteric fractures treated with a compressive hip screw. Hip Int. 2010. 20:221–228.
Article10. Hsueh KK, Fang CK, Chen CM, Su YP, Wu HF, Chiu FY. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: an evaluation of 937 patients. Int Orthop. 2010. 34:1273–1276.
Article11. Jung HJ, Choi JY, Shin HK, et al. Comparison between results of internal fixation and hemiarthroplasty in unstable intertrochanter fracture of osteoporotic bone. J Korean Fract Soc. 2007. 20:291–296.
Article12. Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979. 61:216–221.
Article13. Lee PC, Yu SW, Hsieh PH, Chuang TY, Tai CL, Shih CH. Treatment of early cut-out of a lag screw using a trochanter supporting plate: 11 consecutive patients with unstable intertrochanteric fractures. Arch Orthop Trauma Surg. 2004. 124:119–122.
Article14. Madsen JE, Naess L, Aune AK, Alho A, Ekeland A, Strømsøe K. Dynamic hip screw with trochanteric stabilizing plate in the treatment of unstable proximal femoral fractures: a comparative study with the Gamma nail and compression hip screw. J Orthop Trauma. 1998. 12:241–248.
Article15. Min BW, Lee KJ. Treatment of intertrochanteric fracture: dynamic hip screw. J Korean Fract Soc. 2009. 22:51–55.
Article16. Mulholland RC, Gunn DR. Sliding screw plate fixation of intertrochanteric femoral fractures. J Trauma. 1972. 12:581–591.
Article17. Rha JD, Kim YH, Yoon SI, Park TS, Lee MH. Factors affecting sliding of the lag screw in intertrochanteric fractures. Int Orthop. 1993. 17:320–324.
Article18. Thomas AP. Dynamic hip screws that fail. Injury. 1991. 22:45–46.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subcapital Stress Fracture of the Femur after Internal Fixation of Intertrochanteric Fracture: A case report
- Injury of the Superficial Femoral Artery Secondary to an Unstable Intertrochanteric Fracture: A Case Report
- Fixation Failure after internal Fixation in Intertrochanteric Fractures
- Treatment of intertrochanteric fractures with bipolar hemiarthroplasty in the elderly
- Predictors for Ambulatory Recovery after Fixation of Intertrochanteric Fracture with Proximal Femoral Nail in the Elderly