J Korean Orthop Assoc.
2017 Oct;52(5):428-434. 10.4055/jkoa.2017.52.5.428.
Predictors for Ambulatory Recovery after Fixation of Intertrochanteric Fracture with Proximal Femoral Nail in the Elderly
- Affiliations
-
- 1Department of Orthopaedic Surgery, Dong-Eui Medical Center, Busan, Korea. moonkp@hanmail.net
- KMID: 2393515
- DOI: http://doi.org/10.4055/jkoa.2017.52.5.428
Abstract
- PURPOSE
The purpose of this study was to compare with general characteristics affecting ambulatory recovery at one-year after the fixation of intertrochanteric fracture with proximal femoral nail (PFN) of elderly patients over the age of 65 years.
MATERIALS AND METHODS
Between September 2008 and September 2015, 152 patients were diagnosed with femoral intertrochanteric fracture in Dong-Eui Medical Center. Of these patients, 75 were available in this retrospective study. Multivariate linear regression analysis, using a stepwise selection method, were performed to identify the prognostic factors affecting one-year postoperative recovery of ambulatory status, such as pre-injury ambulatory status, gender, age, fracture type, associated underlying disease, American Society of Anesthesiologists (ASA) grade, dementia, and complication.
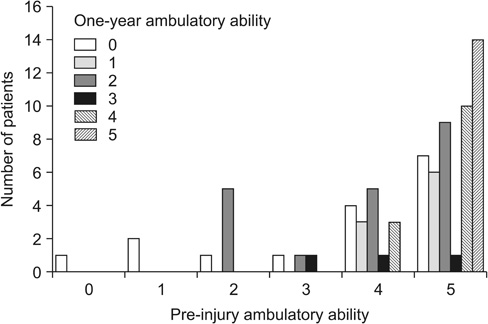
RESULTS
A decrease in the one-year postoperative ambulatory status was 68% and pre-injury ambulatory status was regained in 32% of patients. The pre-injury ambulatory status was the most important determinant of one-year postoperative recovery of ambulatory status. The ASA grade and complication were also predictors of recovery of ambulatory status.
CONCLUSION
Pre-injury ambulatory status, ASA grade and complication were prognostic factors associated with one-year postoperative recovery of ambulatory status after fixating the intertrochanteric fracture using PFN in elderly patients over the age of 65 years.
Figure
Reference
-
1. Deandrea S, Bravi F, Turati F, Lucenteforte E, La Vecchia C, Negri E. Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta-analysis. Arch Gerontol Geriatr. 2013; 56:407–415.
Article2. Lim JY, Park WB, Oh MK, Kang EK, Paik NJ. Falls in a proportional region population in Korean elderly: incidence, consequences, and risk factors. J Korean Geriatr Soc. 2010; 14:8–17.
Article3. Elliott J, Beringer T, Kee F, Marsh D, Willis C, Stevenson M. Predicting survival after treatment for fracture of the proximal femur and the effect of delays to surgery. J Clin Epidemiol. 2003; 56:788–795.
Article4. Schrøder HM, Erlandsen M. Age and sex as determinants of mortality after hip fracture: 3,895 patients followed for 25-18.5 years. J Orthop Trauma. 1993; 7:525–531.5. Ceder L, Thorngren KG, Wallden B. Prognostic indicators and early home rehabilitation in elderly patients with hip fractures. Clin Orthop Relat Res. 1980; 152:173–184.
Article6. Gdalevich M, Cohen D, Yosef D, Tauber C. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg. 2004; 124:334–340.7. Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL. Functional outcomes and mortality vary among different types of hip fractures: a function of patient characteristics. Clin Orthop Relat Res. 2004; 425:64–71.8. Davis FM, Woolner DF, Frampton C, et al. Prospective, multi-centre trial of mortality following general or spinal anaesthesia for hip fracture surgery in the elderly. Br J Anaesth. 1987; 59:1080–1088.
Article9. Clague JE, Craddock E, Andrew G, Horan MA, Pendleton N. Predictors of outcome following hip fracture. Admission time predicts length of stay and in-hospital mortality. Injury. 2002; 33:1–6.
Article10. Ariza-Vega P, Jiménez-Moleón JJ, Kristensen MT. Non-weight-bearing status compromises the functional level up to 1 yr after hip fracture surgery. Am J Phys Med Rehabil. 2014; 93:641–648.
Article11. Fukui N, Watanabe Y, Nakano T, Sawaguchi T, Matsushita T. Predictors for ambulatory ability and the change in ADL after hip fracture in patients with different levels of mobility before injury: a 1-year prospective cohort study. J Orthop Trauma. 2012; 26:163–171.12. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995; 310:150–159.13. Koval KJ, Zuckerman JD. Functional recovery after fracture of the hip. J Bone Joint Surg Am. 1994; 76:751–758.
Article14. Koval KJ, Skovron ML, Polatsch D, Aharonoff GB, Zuckerman JD. Dependency after hip fracture in geriatric patients: a study of predictive factors. J Orthop Trauma. 1996; 10:531–535.
Article15. Lloyd BD, Williamson DA, Singh NA, et al. Recurrent and injurious falls in the year following hip fracture: a prospective study of incidence and risk factors from the Sarcopenia and Hip Fracture study. J Gerontol A Biol Sci Med Sci. 2009; 64:599–609.
Article16. Feng M, Zhang J, Shen H, Hu H, Cao L. Predictors of prognosis for elderly patients with poststroke hemiplegia experiencing hip fractures. Clin Orthop Relat Res. 2009; 467:2970–2978.
Article17. Kauffman TL, Albright L, Wagner C. Rehabilitation outcomes after hip fracture in persons 90 years old and older. Arch Phys Med Rehabil. 1987; 68:369–371.18. Chung YK, Hwang JH, Kim HK. The treatment of peritrochanteric fracture of femur with proximal femoral nail: comparative study with dynamic hip screw. J Korean Hip Soc. 2007; 19:167–175.
Article19. Simmermacher RK, Ljungqvist J, Bail H, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury. 2008; 39:932–939.
Article20. Chang SA, Cho YH, Byun YS, Han JH, Park JY, Lee CY. The treatment of trochanteric femoral fracture with using proximal femoral nail antirotation (PFNA). J Korean Hip Soc. 2009; 21:252–256.
Article21. Liu Y, Tao R, Liu F, et al. Mid-term outcomes after intramedullary fixation of peritrochanteric femoral fractures using the new proximal femoral nail antirotation (PFNA). Injury. 2010; 41:810–817.
Article22. Vochteloo AJ, Moerman S, Tuinebreijer WE, et al. More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int. 2013; 13:334–341.
Article23. Koval KJ, Skovron ML, Aharonoff GB, Zuckerman JD. Predictors of functional recovery after hip fracture in the elderly. Clin Orthop Relat Res. 1998; 348:22–28.
Article24. Kristensen MT. Factors affecting functional prognosis of patients with hip fracture. Eur J Phys Rehabil Med. 2011; 47:257–264.25. Poplingher AR, Pillar T. Hip fracture in stroke patients. Epidemiology and rehabilitation. Acta Orthop Scand. 1985; 56:226–227.26. Mulley G, Espley AJ. Hip fracture after hemiplegia. Postgrad Med J. 1979; 55:264–265.
Article27. Lavelle EA, Cheney R, Lavelle WF. Mortality prediction in a vertebral compression fracture population: the ASA physical status score versus the Charlson Comorbidity Index. Int J Spine Surg. 2015; 9:63.
Article28. Ishida Y, Kawai S, Taguchi T. Factors affecting ambulatory status and survival of patients 90 years and older with hip fractures. Clin Orthop Relat Res. 2005; 436:208–215.
Article29. Lee KJ, Min BW, Kim SG, Song KS, Bae KC, Cho CH. Results of treating senile osteoporotic peritrochanteric fracture with proximal femoral nail antirotation (PFNA). J Korean Hip Soc. 2009; 21:162–168.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ambulatory Recovery after Fixation of Intertrochanteric Fracture with Gamma nail in the Elderly
- Fixation Failure of Proximal Femoral Nail Anti-rotation in Femoral Intertrochanteric Fracture
- Proximal Femoral Nail(PFN) for Femur Intertrochanteric Fracture
- Comparison of the Gamma Nail and the Proximal Femoral Nail in the Treatment of Intertrochanteric Fracture
- Treatment of Intertrochanteric Fracture of Femur: A Randomized Prospective Comparative Analysis of the Internal Fixation of Gamma Nail and Compression Hip Screw