J Korean Neurotraumatol Soc.
2011 Apr;7(1):19-23. 10.13004/jknts.2011.7.1.19.
Availabilities of Cranioplasty with Autologous Bone Flap Preserved within Abdominal Subcutaneous Tissue after Decompressive Craniectomy
- Affiliations
-
- 1Department of Neurosurgery, Chungbuk National University School of Medicine & Medical Research Institute, Cheongju, Korea. dhkim@chungbuk.ac.kr
- KMID: 1427648
- DOI: http://doi.org/10.13004/jknts.2011.7.1.19
Abstract
OBJECTIVE
Autologous cranial bone flap can be preserved either by freezing or by placing in patient's own subcutaneous pocket. The aim of this study is to assess the effectiveness and safety of cranioplasty using an autologous bone flap preserved in a subcutaneous pocket in the patient's own abdominal wall.
METHODS
Twelve autologous bone flaps were preserved in patient's own abdominal subcutaneous pocket between January 2008 and January 2010 at Chungbuk National University Hospital. Two patients who died before cranioplasty due to severe postoperative brain swelling were excluded. We retrospectively reviewed the chart of 10 patients regarding following parameters; age, sex, Glascow Coma Scale score, Glascow Outcome Scale score, cause of craniectomy, interval between craniectomy and cranioplasty and complication.
RESULTS
The cause of craniectomy were severe traumatic brain injury in 9 patients and cerebral infarction in one patient. All of them received unilateral frontotemporoparietal craniectomy, 4 in left side and 6 in right side. The bone flap had been stored in the abdominal wall for an average period of 71 days. There was no postoperative infection or nonunion. All the cases were cosmetically satisfactory. Postoperative subdural fluid collection were developed in 3 cases and one of them underwent revision.
CONCLUSION
We found cranioplasty using autologous bone flap preserved in abdominal wall is safe and effective. Compared to heterologous bone flap and freezing method, autologous bone flap is inexpensive and simple option that preserves the viability of the bone flap. Also, it showed excellent cosmetic results.
MeSH Terms
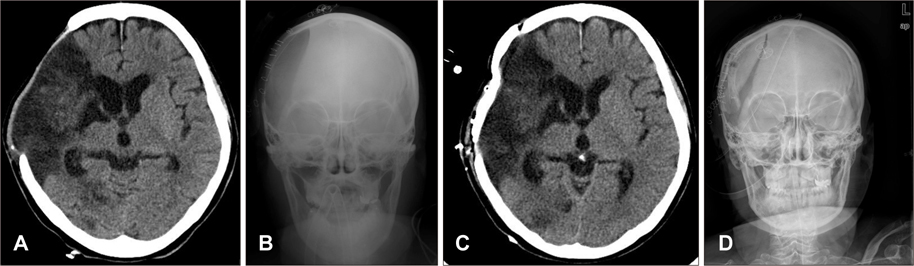
Figure
Reference
-
1. Andrei FJ, Armando L, Evandro DO, Feres CN, João PM. Bone flap management in neurosurgery. Rev Neurocienc. 2009; 17:133–137.
Article2. Baldo S, Tacconi L. Effectiveness and safety of subcutaneous abdominal preservation of autologous bone flap after decompressive craniectomy: a prospective pilot study. World Neurosurg. 2010; 73:552–556.
Article3. Bok WK, Hong SK, Min KS, Lee MS, Kim YG, Kim DH. Cranioplasty using frozen autologous bone. J Korean Neurosurg Soc. 2003; 33:166–169.4. Cho KG, Lee KS. Cranioplasty Using Hydroxylapatite. J Korean Neurosurg Soc. 1990; 19:1009–1014.5. Cho KS, Huh PW, Kim DS, Kim JG, Kim YW, Yoo DS, et al. The infection rate in case of cranioplasty according to used materials and skull defect duration. J Korean Neurosurg Soc. 2001; 30:Suppl 2. 216–220.6. Courtemanche AD, Thompson GB. Silastic cranioplasty following cranio-facial injuries. Plast Reconstr Surg. 1968; 41:165–170.
Article7. Cushing H. The establishment of cerebral hernia as a decompressive measure for inaccessible brain tumors with the description of intramuscular methods of making the bone defect in temporal and occipital regions. Surg Gynecol Obstet. 1905; 1:297–314.8. Dujovny M, Aviles A, Agner C, Fernandez P, Charbel FT. Cranioplasty: cosmetic or therapeutic? Surg Neurol. 1997; 47:238–241.
Article9. Ellis E 3rd, Sinn DP. Use of homologous bone in maxillofacial surgery. J Oral Maxillofac Surg. 1993; 51:1181–1193.
Article10. Goldberg VM, Stevenson S. Natural history of autografts and allografts. Clin Orthop Relat Res. 1987; 225:7–16.
Article11. Gooch MR, Gin GE, Kenning TJ, German JW. Complications of cranioplasty following decompressive craniectomy: analysis of 62 cases. Neurosurg Focus. 2009; 26:E9.
Article12. Häuptli J, Segantini P. [New tissue preservation method for bone flaps following decompressive craniotomy]. Helv Chir Acta. 1980; 47:121–124.13. Hwang KH, Kim TY, Kim JM. Autogenous cranioplasty using deep-freezing bone flap. J Korean Neurosurg Soc. 1998; 27:159–164.14. Koh MS, Goh KY, Tung MY, Chan C. Is decompressive craniectomy for acute cerebral infarction of any benefit? Surg Neurol. 2000; 53:225–230.
Article15. Krishnan P, Bhattacharyya AK, Sil K, De R. Bone flap preservation after decompressive craniectomy--experience with 55 cases. Neurol India. 2006; 54:291–292.16. Kulali A, Kayaalp S. Single-table autogenous calvarial grafting for cranioplasty. J Craniomaxillofac Surg. 1991; 19:208–211.
Article17. Movassaghi K, Ver Halen J, Ganchi P, Amin-Hanjani S, Mesa J, Yaremchuk MJ. Cranioplasty with subcutaneously preserved autologous bone grafts. Plast Reconstr Surg. 2006; 117:202–206.
Article18. Park JY, Seok KS, Cho JH, Kang DG, Kim SC. Early decompressive craniectomy for cerebral edema. J Korean Neurosurg Soc. 2002; 31:33–38.19. Schwab S, Steiner T, Aschoff A, Schwarz S, Steiner HH, Jansen O, et al. Early hemicraniectomy in patients with complete middle cerebral artery infarction. Stroke. 1998; 29:1888–1893.
Article20. Tabaddor K, LaMorgese J. Complication of a large cranial defect. Case report. J Neurosurg. 1976; 44:506–508.21. Winkler PA, Stummer W, Linke R, Krishnan KG, Tatsch K. Influence of cranioplasty on postural blood flow regulation, cerebrovascular reserve capacity, and cerebral glucose metabolism. J Neurosurg. 2000; 93:53–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison with Subcutaneous Abdominal Preservation and Cryoconservation Using Autologous Bone Flap after Decompressive Craniectomy
- Delayed and recurrent surgical site infection from resorbed bone fragment after autologous cranioplasty: a case report
- Analysis of Cranioplasty Using Frozen Autologous Bone Following Post-Traumatic Decompressive Craniectomy
- Bone Resorption of Autologous Cranioplasty Following Decompressive Craniectomy in Children: Case Report
- Cranioplasty Using Frozen Autologous Bone