J Korean Surg Soc.
2013 Sep;85(3):104-108. 10.4174/jkss.2013.85.3.104.
On-site ultrasound-guided localization for impalpable nodal recurrences in papillary thyroid carcinoma patients
- Affiliations
-
- 1Department of Surgery, The Armed Forces Capital Hospital, Seongnam, Korea.
- 2Thyroid Cancer Center, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. surghsc@yuhs.ac
- KMID: 1426341
- DOI: http://doi.org/10.4174/jkss.2013.85.3.104
Abstract
- PURPOSE
The cervical lymph nodes are the most common sites of locoregional recurrence in patients with papillary thyroid carcinoma (PTC). Accurate tumor localization is important for the successful removal of impalpable recurrences in the cervical lymph nodes. We evaluated the benefits of ultrasound-guided localization (UGL) performed by a single surgeon on site.
METHODS
Of 53 PTC patients who underwent reoperation for impalpable nodal recurrences, 32 (group 1) were assessed only using preoperative imaging, while 21 (group 2) were additionally evaluated by on-site UGL performed by the operating surgeon. Postoperative outcomes were compared between the two groups.
RESULTS
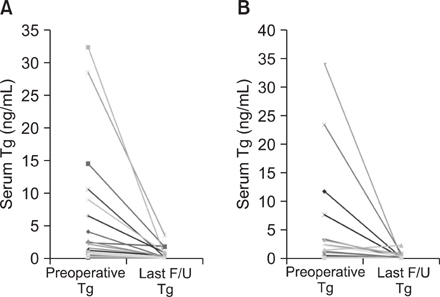
Operation times were significantly shorter (P < 0.001) and the mean size of the resected lymph nodes were smaller (P = 0.013) for group 2 patients. More lymph nodes were identified and resected in group 1 (3.56 vs. 3.19), but the rate of positive lymph nodes was significantly higher in group 2 (P < 0.001). There were no differences between the two groups in terms of resection success rate, complication rate, and postoperative hospital stay. During a mean follow-up period of 27.6 months, 52 patients (98.1%) showed no evidence of recurrence on routine ultrasound, and serum thyroglobulin concentrations remained < 1 ng/mL in 49 patients (92.5%).
CONCLUSION
On-site UGL performed by the operating surgeon is useful for accurate resection of impalpable nodal recurrences in PTC patients.
MeSH Terms
Figure
Reference
-
1. Caron NR, Clark OH. Well differentiated thyroid cancer. Scand J Surg. 2004; 93:261–271.2. Schlumberger MJ. Papillary and follicular thyroid carcinoma. N Engl J Med. 1998; 338:297–306.3. Mazzaferri EL, Kloos RT. Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab. 2001; 86:1447–1463.4. Cobin RH, Gharib H, Bergman DA, Clark OH, Cooper DS, Daniels GH, et al. American Association of Clinical Endocrinologists. American College of Endocrinology. AACE/AAES medical/surgical guidelines for clinical practice: management of thyroid carcinoma. Endocr Pract. 2001; 7:202–220.5. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006; 16:109–142.6. Schlumberger M, Pacini F, Wiersinga WM, Toft A, Smit JW, Sanchez Franco F, et al. Follow-up and management of differentiated thyroid carcinoma: a European perspective in clinical practice. Eur J Endocrinol. 2004; 151:539–548.7. Frasoldati A, Pesenti M, Gallo M, Caroggio A, Salvo D, Valcavi R. Diagnosis of neck recurrences in patients with differentiated thyroid carcinoma. Cancer. 2003; 97:90–96.8. Pacini F, Molinaro E, Castagna MG, Agate L, Elisei R, Ceccarelli C, et al. Recombinant human thyrotropin-stimulated serum thyroglobulin combined with neck ultrasonography has the highest sensitivity in monitoring differentiated thyroid carcinoma. J Clin Endocrinol Metab. 2003; 88:3668–3673.9. Goretzki PE, Simon D, Frilling A, Witte J, Reiners C, Grussendorf M, et al. Surgical reintervention for differentiated thyroid cancer. Br J Surg. 1993; 80:1009–1012.10. Gemsenjager E, Perren A, Seifert B, Schuler G, Schweizer I, Heitz PU. Lymph node surgery in papillary thyroid carcinoma. J Am Coll Surg. 2003; 197:182–190.11. Cross S, Wei JP, Kim S, Brams DM. Selective surgery and adjuvant therapy based on risk classifications of well-differentiated thyroid cancer. J Surg Oncol. 2006; 94:678–682.12. Alzahrani AS, Raef H, Sultan A, Al Sobhi S, Ingemansson S, Ahmed M, et al. Impact of cervical lymph node dissection on serum TG and the course of disease in TG-positive, radioactive iodine whole body scan-negative recurrent/persistent papillary thyroid cancer. J Endocrinol Invest. 2002; 25:526–531.13. Chao TC, Jeng LB, Lin JD, Chen MF. Reoperative thyroid surgery. World J Surg. 1997; 21:644–647.14. Dralle H, Sekulla C, Haerting J, Timmermann W, Neumann HJ, Kruse E, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004; 136:1310–1322.15. Salvatori M, Rufini V, Reale F, Gajate AM, Maussier ML, Revelli L, et al. Radio-guided surgery for lymph node recurrences of differentiated thyroid cancer. World J Surg. 2003; 27:770–775.16. Karwowski JK, Jeffrey RB, McDougall IR, Weigel RJ. Intraoperative ultrasonography improves identification of recurrent thyroid cancer. Surgery. 2002; 132:924–928.17. Kang TW, Shin JH, Han BK, Ko EY, Kang SS, Hahn SY, et al. Preoperative ultrasound-guided tattooing localization of recurrences after thyroidectomy: safety and effectiveness. Ann Surg Oncol. 2009; 16:1655–1659.18. Triponez F, Poder L, Zarnegar R, Goldstein R, Roayaie K, Feldstein V, et al. Hook needle-guided excision of recurrent differentiated thyroid cancer in previously operated neck compartments: a safe technique for small, nonpalpable recurrent disease. J Clin Endocrinol Metab. 2006; 91:4943–4947.19. McCoy KL, Yim JH, Tublin ME, Burmeister LA, Ogilvie JB, Carty SE. Same-day ultrasound guidance in reoperation for locally recurrent papillary thyroid cancer. Surgery. 2007; 142:965–972.20. Mazzaferri EL, Robbins RJ, Spencer CA, Braverman LE, Pacini F, Wartofsky L, et al. A consensus report of the role of serum thyroglobulin as a monitoring method for low-risk patients with papillary thyroid carcinoma. J Clin Endocrinol Metab. 2003; 88:1433–1441.21. Peter C, Hongwan D, Kupfer A, Lauterburg BH. Pharmacokinetics and organ distribution of intravenous and oral methylene blue. Eur J Clin Pharmacol. 2000; 56:247–250.22. Fukui Y, Yamakawa T, Taniki T, Numoto S, Miki H, Monden Y. Sentinel lymph node biopsy in patients with papillary thyroid carcinoma. Cancer. 2001; 92:2868–2874.23. Tuttle TM. Technical advances in sentinel lymph node biopsy for breast cancer. Am Surg. 2004; 70:407–413.24. Patel HP, Chadwick DR, Harrison BJ, Balasubramanian SP. Systematic review of intravenous methylene blue in parathyroid surgery. Br J Surg. 2012; 99:1345–1351.25. Shah-Khan MG, Lovely J, Degnim AC. Safety of methylene blue dye for lymphatic mapping in patients taking selective serotonin reuptake inhibitors. Am J Surg. 2012; 204:798–799.26. Gillman PK. CNS toxicity involving methylene blue: the exemplar for understanding and predicting drug interactions that precipitate serotonin toxicity. J Psychopharmacol. 2011; 25:429–436.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound (US)-Guided Ablation of Thyroid Nodules
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- Coexistence of Parathyroid and Papillary Thyroid Carcinoma
- Oxyphilic Papillary Carcinoma of the Thyroid in Fine Needle Aspiration
- Ultrasound-guided radiofrequency ablation for the treatment of papillary thyroid carcinoma: a review of the current state and future perspectives